Environmental contamination associated with biofuel production involving pesticide-coated
April 6, 2025
- Research
- Open access
- Published: 07 April 2025
Environmental Health
volume 24, Article number: 17 (2025)
Abstract
A United States ethanol company used pesticide-coated seed corn for fuel ethanol production, resulting in highly contaminated byproducts. Improper storage and disposal of the waste led to widespread environmental contamination. Detectable levels of neonicotinoids have been found in soil, water, and air samples, raising questions about the potential impacts to the environment and human health. The study objective was to evaluate the community’s perceived physical and mental health impacts and needs resulting from the contamination linked to bioenergy production by a single company.
A 54-question survey was administered to households located within a 10-mile radius of the facility. Respondents could complete the paper survey and return it by mail or electronically. The general topics were household members’ awareness, concerns, and perceptions of environmental and health impacts. Quantitative data were presented as frequencies and percentages, while qualitative data were grouped into themes based on keywords and summarized as counts.
A total of 459 respondents completed the survey, a 38% response rate. The average household size was 2.7 (SD = 1.4). Responding households were primarily single-family homes (89%) that were owned (85%), and were long-time residents (mean = 18.4 years, SD = 15.5). A total of 36% of households included children aged 18 or younger. Respondents were concerned about contaminants affecting water (82%), soil (79%), and air (72%) quality. Most respondents (74%) felt some or a lot of stress related to potentially compromised health; however, 51% did not believe they had health symptoms resulting from the contamination. The most common self-reported symptoms among primary respondents were sinus (n = 17), respiratory (n = 22), cognitive/neurological symptoms (n = 15), and allergies (n = 17). Depression and anxiety were the primary mental health symptoms reported with 31 mentions. The top community need was wanting the environment cleaned-up, including proper removal of waste and land restoration.
This study evaluated community-level perceived impacts of environmental contamination directly related to an ethanol plant’s improper handling of production waste containing pesticides. Findings can support immediate actions by state officials and community leaders and serve as a baseline for future health and environmental monitoring.
Background
Rural economies in the central United States (U.S.) largely depend on agriculture [1]. Corn and biofuel production is concentrated in the Midwest, with three states (IA, NE, IL) contributing half of all domestically produced corn and fuel ethanol [2]. Seed companies introduced seeds that were pre-treated with insecticides and fungicides in the mid-2000s, and now coated seeds account for 90% of all seed corn sold in the U.S [3, 4]. Neonicotinoids are a popular class of pesticide used in the U.S. and commonly used as seed coatings. While the pesticide-treated seeds are an unregulated product, there are regulatory and nonregulatory standards for individual neonicotinoid (neonic) concentrations in the environment set by the U.S. Environmental Protection Agency (EPA) [5,6,7]. Thus, the potential human and environmental health impacts directly tied to the wide-spread use of treated seeds in the agricultural industry is unknown [3, 8]. In 2021, Nebraska banned [9] using treated seed for ethanol production, following the forced closure of an ethanol plant that used excess treated seed obtained from seed companies for ethanol production instead of the industry standard, field corn.
AltEn, LLC, an ethanol production facility located in rural Nebraska about 20 miles west of Omaha produced an estimated 24 million gallons of ethanol per year [10]. In 2015, the company switched to using leftover seed corn coated with fungicides and pesticides (such as neonicotinoids) for fuel ethanol production. Processing the pesticide-treated seeds during production resulted in heavily contaminated byproducts (solid and liquid waste and distillers grain, also known as, wet cake) which eventually led to environmental contamination because of improper disposal and waste management practices [8, 11]. Due to legal compliance issues and community concerns, AltEn was forced to close in February 2021 after operating for seven years.
Environmental sampling found detectable levels of neonics in water, air, and soil samples from the worksite and near and inside homes [8, 11]. Therefore, potential human and animal exposure routes include inhalation, ingestion, and dermal routes. Detectable levels of neonics or a transformed product were found in urine samples from residents living nearby which suggested exposures were still occurring because the water soluble compounds are quickly eliminated [12]. The sources of environmental contamination stemmed from the plant and surrounding farmland that had been treated with contaminated wastewater. Further, AltEn had 150,000,000 gallons of wastewater stored in lagoons and 84,000 tons of solid waste or wet cake onsite [11, 13]. The lagoons were lined to protect the pesticide-contaminated wastewater from reaching ground water. However, tears in the lagoon lining, stormwater runoff, and two large spills, occurring in February and September 2021, threatened water quality [10]. The levels of neonics in the wastewater and wet cake were found to far exceed EPA standards, as early as 2019 [8]. Lastly, there was potential for particulate matter from the treated agricultural soil or piles of wet cake to impact air quality. Testing is ongoing to evaluate how much of the contamination can be linked to AltEn activities since the presence of neonics in the environment is expected because of the agricultural activity in the area.
Neonicotinoids are insecticides commonly used in agricultural production, landscaping, and flea and tick prevention for domestic pets [3]. Human populations can be exposed to neonics through a variety of sources including occupational or domestic use, water, diet, and previously treated soil or dust [14,15,16,17,18]. A recent study using 2015–2016 National Health and Nutrition Examination Survey (NHANES) data, considered to be representative of the U.S. general population, found 49% of respondents had been recently exposed to neonics based on having detectable levels of at least one of six urinary biomarkers (i.e., parent compound or metabolite) [14]. While this study provides some basis for understanding exposures in the general population, there is potential for agricultural communities to have greater exposure to neonics and other agricultural chemicals involved in food and animal production [15]. It is not known if these communities experience a disproportionate health burden specifically related to neonics.
Epidemiologic studies of the human health effects of neonic exposure are scarce [3, 19,20,21,22]. Most of the available evidence relates to imidacloprid exposures or general exposure to pesticides including neonics [19]. Acute exposures from neonic poisonings (unintentional and intentional) have been associated with a range of mild to moderate symptoms including nausea, vomiting, headache, and dizziness [23, 24]. A recent scoping review was conducted by the National Toxicology Program to summarize scientific evidence on chronic low-level exposures to neonics and human health outcomes [19]. Of the 25 publications meeting the study inclusion criteria, only six were epidemiologic studies (e.g., case-control (n = 5) or cross-sectional (n = 1)), with the rest being case reports, and none were conducted in the Midwestern United States where agricultural production is prevalent [19]. The scoping review included animal and human studies and found overall, congenital/development or neurological outcomes were the most frequently studied [19]. However, the resulting conclusions were hindered by the heterogeneity across studies [19]. For example, different health outcomes and neonic compounds were evaluated, misclassification of exposure was likely based on the study methodology, and there was inadequate control for confounding in analyses. Furthermore, there is very little evidence on relationships between agricultural and occupational neonic exposures and health outcomes. In a small (n = 19) case-crossover occupational study, Swedish conifer farmers were exposed to seeds treated with imidacloprid, and symptoms were reported during a control window (a week handling untreated seeds) and 1-week following planting of the neonic-treated seeds [25]. Of the six planters that experienced symptoms in the week following planting with neonic-coated seeds but not during the control week, irritated or blocked nose were the symptoms most frequently reported [25].
Given the limited research on the human health effects of neonic exposures in the United States and the unique contamination and exposure scenario resulting from AltEn practices, it was important to gain community insight into the perceived impacts on the environment and to local residents’ physical and mental health. Therefore, this study addressed the following research questions: (1) what are the community’s perceived physical and mental health effects related to AltEn ethanol plant activities, and (2) what are the community’s environmental concerns and needs following the closure of AltEn? The results from our study characterize a community’s perspective following a contamination event and support further investigation into neonic and health relationships.
Methods
In this cross-sectional study, the target population included all residential addresses located within a 10-mile radius from the AltEn plant (n = 977). In addition, six former AltEn employees, and the general public were invited to complete the survey. Out of 977 household addresses sampled, 2.1% (n = 21) were ineligible (no such address; vacant) and 0.8% (n = 8) were undeliverable addresses with unknown eligibility. Seven addressees (0.7%) refused to participate in the survey as indicated by a blank survey returned, letter, phone call, email, or refused mail. Two screener questions were used to ensure that an adult completed the survey (Appendix A).
The 54-item survey evaluated primary household respondent and household members’ awareness, concerns and perceptions of environmental and health impacts resulting from AltEn ethanol plant operations. The University of Nebraska Lincoln Bureau of Sociological Research (BOSR) consulted on survey questions and administered the household survey. Respondents had the opportunity to complete the survey by mail and via the Internet. Data collection was initiated on February 16, 2022, and closed on May 26, 2022. Initially, residents were sent a packet including a cover letter, web link to online survey, information about AltEn situation, and a notepad incentive. Additionally, we used a separate referral card (online survey) to determine if respondents would like to be contacted in the future for participation in biological (human blood, urine), animal (livestock or pet samples), or environmental (soil, water, air) sampling, or to be contacted by an occupational health specialist. A total of three reminders were mailed to survey non-respondents at one, three and four weeks post-initial mailing. The first and second reminders included the cover letter and electronic survey link, and the final reminder included a paper survey with two postage-paid return envelopes and a paper referral card. The six previous AltEn employees were emailed the initial survey invitation on February 28, 2022. We emailed the initial survey invitation to the six previous AltEn employees on February 28, 2022. BOSR sent a single reminder email on March 9, 2022, to all prior employees that had not completed the survey. At the end of March 2022, the public survey was made available on the UNMC AltEn information webpage and passively collected responses for two months. The public survey was anonymous but included questions to ensure duplicate responses from the study sample could be identified and removed. The study was approved by the University of Nebraska Medical Center Institutional Review Board (IRB).
Paper survey responses were entered into a database using SurVADE software by trained and experienced data entry staff at BOSR. Each survey was entered twice by independent data entry staff. Discrepancies between entries were reviewed and resolved with the help of a supervisor. Web surveys utilized Qualtrics for data collection. Responses across survey mode were combined using SPSS and duplicate entries (e.g. a household responded to both the mail survey and web survey) were removed. Next, the responses from the public survey and AltEn employee survey were merged into a single database. The data were checked for quality using simple descriptive statistics and open-ended/qualitative responses were reviewed for completeness.
Household survey responses were summarized using frequencies and percentages. The open-ended, qualitative responses were coded into general themes and frequencies were presented. Two researchers independently reviewed the text responses and grouped them into themes. Then, the study team met to review the findings and resolve any differences. For health symptom responses, the keyword was counted and assigned to a group to describe frequency of mentions. For example, a single respondent might have listed several symptoms such as allergies, headaches, and sore throat resulting in three symptoms counted and categorized. Supplemental Table 1 shows the keywords included in each symptom category. Quantitative analyses were conducted using SAS v9.4 (Cary, NC).
Results
The analysis included responses from 459 survey respondents from community residents (n = 372), the general public (n = 84), and former AltEn employees (n = 3); response rate 37.8%. A small proportion of addresses were ineligible (n = 29, 3%) and seven refusals were received (0.7%). From Table 1, most respondents lived in a single-family home (89%), were homeowners (85%), and were long-time residents, over 18 years on average. The average household size was 2.7. Households included members from all age groups, ranging from infants to elderly adults over the age of 65. Specifically, the percentage of households that had at least one member in the following age groups are: 0–2 years (4%), 2–11 years (16%), 12–18 years (16%), 19–34 (19%), 35–65 (61%), and over the age of 65 (28%).
Three survey questions assessed community members’ awareness and sources of public information (Table 2). The majority of respondents (n = 370, 81%) had heard about the AltEn situation prior to receiving the study survey. Respondents first learned about the AltEn situation primarily through living nearby and word of mouth either through neighbors, AltEn employees, or their local employer (n = 72, 16%). Other common sources were social media (n = 70, 15%) or TV (n = 66, 14%). To stay informed, respondents indicated that they received information about the AltEn situation from TV (n = 95, 21%), newspaper (n = 65, 14%), or social media (n = 56, n = 12%). Other less frequently mentioned information sources were radio, internet source other than social media, and word of mouth.
The survey included several questions about environmental concerns related to AltEn activities and potential environmental exposures based on living and working conditions and habits. Most survey respondents (n = 343, 75%) indicated their household was concerned about the AltEn situation (Table 2). Among the households that were concerned, 50% reported being very concerned, and nearly 50% were somewhat concerned. Respondents were also asked to rate their level of stress (no stress, some stress, a lot of stress) for the following categories: compromised health, feeling overlooked by decision makers, financial worry, and feeling the crisis will never be fixed. Most households felt at least some stress across all categories. Feeling the crisis would never be fixed (50%) and having been overlooked by decision makers (41%) were the most frequent causes of ‘a lot of stress’ among worried households. Compromised health led to a reported 22% of respondents feeling ‘a lot of stress’ and another 52% ‘some stress’. Respondents self-reported a range of other drivers of stress including environmental impacts, human and animal health, property values, and plans for the clean-up.
The survey asked about animal ownership and health (Table 3). The majority (73%) of households had a pet(s) with 38% living indoors only, 14% outdoors only or went between indoors and outdoors 47.5%. Furthermore, 19% of households owned livestock. Some respondents accessed veterinary care for pets (85%) or livestock (36%). Animal symptoms were provided by 9 households and included the keywords cancer, neurological, extreme itching, vomiting, constant cough and cold symptoms, hair loss, loss of function in rear legs.
The survey also included questions related to environmental impact concerns including air quality, smell, surface water contamination, well water quality, wet cake application, and soil contamination. Most households were concerned about all stated environmental factors, with more than 80% concerned about well water quality and surface water contamination (Table 4).
The primary sources of drinking water were private well water (55%) and bottled water (45%). Several households relied on filtered municipal tap water for drinking water (n = 107, 23%). The most common filters were refrigerator (n = 48), kitchen sink (n = 32), pitcher (n = 26) and water valve/whole house filter (n = 21). Among all respondents, 74 indicated their main source of drinking water had changed since 2015. Some of the most common reasons included concerns about AltEn activities or water contamination in general (e.g., switching to bottled water), discolored or cloudy water and poor taste and/or smell, or moved away. Lastly, most respondents (74%) had direct contact with soil or dust through work, hobbies or other activities indicating some level of exposure to these outdoor sources.
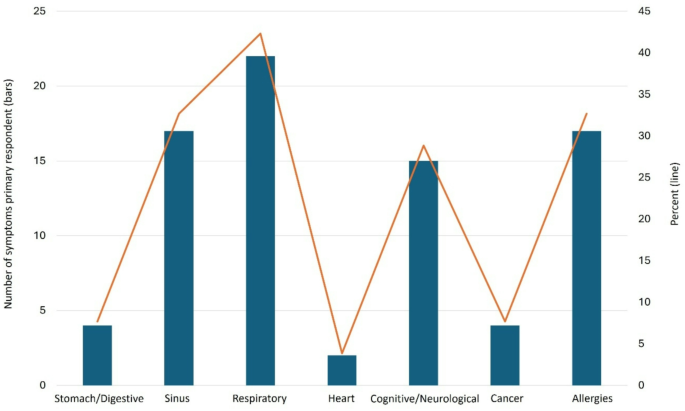
We evaluated physical health symptoms of primary respondents using the following question, “Since 2015, have you experienced any health issues that you felt were related to the activities at the AltEn plant?”. Half of the primary respondents (n = 234, 51%) answered ‘no’, while 39% (n = 178) responded ‘yes’ (n = 52, 11.3%) or ‘unknown’ (126, 27.5%) to the question (no response n = 47, 10.2%). Figure 1 displays the number and percentage of self-reported symptoms within each health category. Symptoms related to respiratory (n = 22, e.g., asthma, cough), allergies (n = 17, e.g., allergies, sneezing), sinuses (n = 17, e.g., bloody nose, sinus pain or infection, runny nose), and cognitive/neurological (n = 15, e.g., headaches, migraines) systems were the most frequently mentioned. Supplementary Table 1. Displays the keywords captured from the open-ended responses and grouped into health categories.
Self-reported physical symptoms among primary survey respondents. Self-reported physical health symptoms from open-ended question (Q33) among primary survey respondents that answered, ‘Yes’ to Q32 “Since 2015, have you experienced any health issues that you felt were related to the activities at the AltEn plant?” n = 52. Figure displays the number of symptoms classified into a health category (bars) and the percent (lines). Multiple symptoms could be described by a single respondent
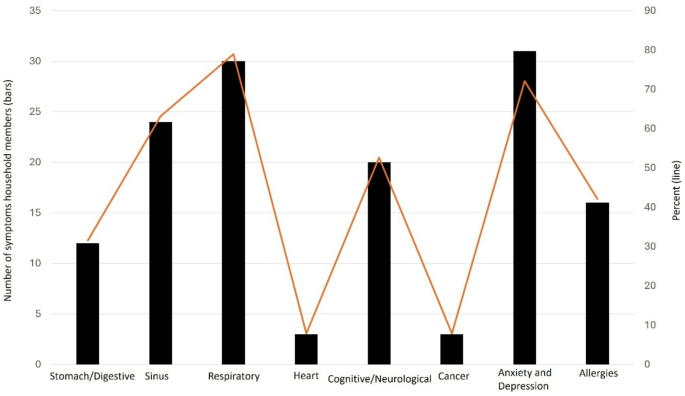
Physical health symptoms were also evaluated for the household members using the following question, “Since 2015, has anyone in your household experienced any health issues they felt were related to the activities at the AltEn plant?”. More than half (n = 250, 54%) answered ‘no’, while 8% answered ‘yes’ (n = 38) or 25.7% ‘unknown’ (n = 118) to the question (no response n = 53, 11.6%). Figure 2 displays the household members’ self-reported symptoms. Regarding mental health, some respondents indicated a member of their household had experienced adverse mental health symptoms related to AltEn activities, responding ‘yes’ (n = 43, 9.4%) or ‘unknown’ (n = 20, 4.4%) to the question, “Starting in 2015, have you or anyone in your household experienced any mental health issues?”. Anxiety and/or depression were the most frequently self-reported mental health symptoms (n = 31, Fig. 2).
Self-reported physical and mental health symptoms– All household members. Self-reported physical and mental health symptoms for each household member (Q37), among primary survey respondents responding ‘Yes’ to the question Q35 “Since 2015, has anyone in your household experienced any health issues they felt were related to the activities at the AltEn plant?” n = 38. Symptoms could be reported for each member of the household separately. Figure displays the number of symptoms classified into a health category (bars) and percentage (line). Household symptoms sample sizes: Member 1 (n = 36), Member 2 (n = 22), Member 3 (n = 9), Member 4 (n = 2), Member 5 (n = 0). Mental health household symptoms “Starting in 2015, have you or anyone in your household experienced any mental heath issues?” (Q43) Yes (n = 43). 40/43 (93%) provided the self-reported mental health system in Q44. Multiple symptoms could be described by a single respondent
Most primary respondents self-reported a symptom onset between 2015 and 2017 (N = 19, 36.5%) or 2018–2020 (N = 22, 42.3%). Lastly, 66 (14%) of households responded yes to any of the substances listed in response to the question, “Since 2015 have you or a member of your household increased the use of tobacco products, alcohol, marijuana, other illicit drugs, or prescription or over the counter drugs not used at directed?”. Specifically, 5% reported increased use of tobacco products, 10% alcohol consumption, 2% marijuana use, 0% other illicit drugs, and 2.6% prescription or over the counter drugs not used as directed.
Most respondents had no difficulty accessing health care since 2015, with 11 (2.4%) reporting difficulty accessing medical care and 385 (83.9%) having no difficulty (no response: n = 63, 13.7%). Similarly, 8 (1.7%) of respondents had difficulty accessing mental health care with the majority (n = 378, 82.4%) experiencing no difficulty (no response n = 73, 15.9%). Barriers to care included lack of insurance, wait times, or lost employment.
Lastly, the survey included two questions regarding pregnancy outcomes. The first question asked, “Since 2015, how many pregnancies, including miscarriages, have occurred in your household?” Most responded zero (n = 143, 31.15%) or not applicable-no women of childbearing age/not trying to have children (n = 268, 58.4%), while 48 (10.5%) had at least one pregnancy. The second question asked, “Since 2015, were any pregnancies miscarried?” to which 13 (2.8%) responded ‘Yes’.
Information on self-reported chronic condition diagnoses was collected by the following question, “Since 2015, have you or a member of your household ever been told by a healthcare professional that you or a member of your household have a chronic (long-term) condition?” The majority answered ‘no’ (n = 293, 64%). Among those answering ‘yes’ (n = 79) or ‘unknown’ (n = 27), 80 respondents self-reported a diagnosis of a chronic disease by a health professional after 2015. The most common were respiratory diseases, including asthma, chronic obstructive pulmonary disease (COPD), chronic cough (combined n = 22), and heart disease (n = 13).
Among respondents that indicated they or a member of their household had been diagnosed by a healthcare professional with a chronic condition, 18 indicated it was a form of cancer. Self-reported cancer sites included breast, prostate, brain, blood, skin, kidney, lung, bladder, head and neck, musculoskeletal and ovarian. All cancer types had a sample size of less than five.
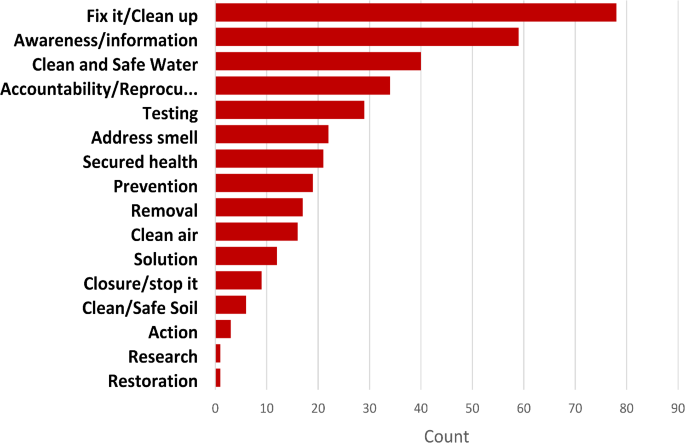
Community needs related to AltEn were collected through an open-ended question. Figure 3 describes the number of responses within each theme (306/459, 67% of respondents). The top three community needs were as follows. (1) Fix it/Clean-up: cleaning the waste and contaminants safely, properly, and quickly (n = 78). Residents were concerned about further contamination of the water, soil, and air, and wondered if their residential environment was safe (i.e., a need for testing and monitoring), (2) Awareness/Information, transparent and clear communication regarding information on current environmental contamination and potential health hazards, and (3) Access to clean and safe water.
Community needs. Community needs identified and coded based on themes. Household respondents were asked to identify their greatest household needs related to AltEn (N = 306)
Respondents were most concerned about the remediation and clean-up of the AltEn site. For example, one respondent commented on removing the wet cake and toxic chemicals: “Needs to be done NOW and not a year from now. There should have been a plan in place before any of this happen[ed].” A second respondent discussed that they had noticed “a lot more sick people in the area” and that “the State and Federal [government] needs to get on board.” A third respondent commented on the inadequacy of previous efforts to cover the waste and smell: “Remove the solid waste from AltEn: covering it (occurred last month) does not help reduce the odor or the runoff/leaching concerns. We are getting very upset with the rate at which this waste product is being removed.”
The second most frequently recognized need was for better communication to increase awareness and sharing of information related to the clean-up and environmental and human health risks. One respondent expressed the need for timely updates to keep community members well informed stating, “frequent ongoing information about what is taking place there regarding health hazards for our community in the future.” Respondents wanted a complete picture on the extent of the contamination, what the associated health risks are and how risks will be mitigated by cleanup efforts. Information was requested from one respondent on “where wet cake was distributed; more information on what the state is doing and what potential impacts are” while another respondent was concerned about contamination around their home writing, “testing of soil, water, and air to confirm whether contamination reached ou[r] property.” Another respondent focused on potential current and future health impacts stating, “seeing how our land and water/animals and health has been affected now and in the future.” The third greatest community need was ensuring access to clean and safe water. Recognizing the ongoing need to monitor water quality in the community a respondent wrote, “I would like to be assured that our drinking water is safe and that future contamination to the surrounding environmental will not result from the clean-up of the facility, while another expressed concern specifically about well water quality writing, “make sure our well water is safe.”
The remaining community need themes were focused on seeking justice (accountability/repercussions), evaluation and environmental testing to understand the extent of the contamination and potential human health impacts, and actions including: addressing the strong smell originating from the byproducts and removing contaminants.
Discussion
The purpose of this study was to assess community environmental and health concerns and needs following the forced closure of the AltEn ethanol plant. Early environmental sampling indicated detectable levels of neonics in outdoor air, water, soil, and residences [8, 11]. Urine samples provided by nearby residents had detectable levels of neonics (or transformed product), suggesting ongoing exposures [12]. The survey was administered one year after the ethanol plant closed and clean-up efforts were ongoing. To our knowledge, this is the first environmental contamination event to occur from an ethanol plant that had used treated seeds for bioenergy production. While the general population likely experiences chronic low-level exposures to neonics [14], this disaster may have resulted in higher acute exposures for nearby residents because of the concentrated levels of neonics in byproducts stored onsite and previously distributed on farmland.
Our study addressed community-level environmental concerns about potential routes of exposure. Respondents reported a high level of concern about environmental contamination, specifically surface and well water. Private wells were the primary source of drinking water for over half of respondents, with only a small percentage changing their drinking water source since AltEn began production with pesticide-coated seeds in 2015. Nearly half of households were using bottled water as their main source of drinking water, further demonstrating community concerns about safe drinking water. Most households were also concerned about soil and air contamination. Half of respondents reported feeling a lot of stress that the crisis would never be fixed. This was also a top community need identified from the survey.
While the ethanol plant was operational, some community members reported concerns about their health or the health of their animals [10]. State testing as early as 2019 indicated high levels of neonics in the byproducts stored on the worksite, and additional evidence of environmental contamination emerged after the closure. Therefore, it was important to capture perceived health symptoms from residents in nearby communities that may have been exposed to neonics and other chemicals from AltEn to inform future monitoring and clean-up efforts. Results indicated most respondents were stressed about the potential for compromised health, though just over one-third reported their health may have been impacted by AltEn activities. The most frequently attributed symptoms were allergies, sinus issues, respiratory (e.g., cough, shortness of breath) and cognitive or neurological symptoms, primarily headaches or migraines. Symptoms relating to gastrointestinal or cardiovascular system, and cancer were less frequently mentioned. The evidence of possible human health effects from neonic exposures is severely limited [3, 19, 20]. Also, the neonic exposure scenario resulting from environmental contamination from AltEn activities is unique and will require future monitoring to understand potential health implications. According to data from national surveys, 26% of adults have seasonal allergies [26] and 12% are affected by chronic sinusitis [27]. Respiratory symptoms can be influenced by many factors (e.g. infections, chronic respiratory disease, allergy, environmental exposures, and weather, etc.).
The prevalence of severe headaches and migraines among adults is 15.3% [28]. Lastly, according to the National Health Interview Survey, the prevalence of mental health symptoms among adults was 18% for anxiety and 21% for depression [29].
This study had some limitations. The survey was conducted a year after the closure of the plant which had been in operation for seven years. Therefore, residents and nearby community members most affected by the plant’s activities and resulting contamination may have moved prior to survey administration, potentially resulting in a failure to capture individuals with severe health symptoms. However, most respondents reportedly lived in their homes for more than 15 years, on average, suggesting many have stayed, and this delay should have resulted in less immediacy bias from the local news coverage surrounding the event around the AltEn plant closure. The study purpose was to collect data on the community’s perceived impacts to their health and local environment, therefore, health symptoms and diagnoses were self-reported in open-ended question format and have not been verified by a health practitioner. A strength of this approach is any health symptom could be mentioned without influence by a predetermined list of possible symptoms. The limitation is it is difficult to compare symptom rates with other survey data due to differences in methodology. The response rate was modest (38%), with less than half of the target population responding to the survey. While this raises some concerns about selection bias and representativeness of findings, our response rate was comparable to other population-based surveys [30] and only 2.9% of addresses were ineligible (n = 29). Seven respondents (0.7%) refused to participate but reasons for refusal/non-response to the survey were not collected. Bias can be introduced if non-respondents are different from survey respondents, but this is difficult to evaluate given the limited information on non-respondents (i.e. mailing address). We compared survey respondents to non-respondents using residential zip code and the proportion of non-response was similar across zip codes. The survey was self-administered and included skip patterns, which likely contributed to item non-response ranging from 1 to 28%. This study also had several strengths including a sampling design where surveys were sent to all residential addresses located in a 10-mile radius around AltEn and public survey to capture most people impacted by AltEn, a range of questions to understand the community’s perspective following an environmental disaster, and timely collection of community data alongside environmental sampling efforts following the plant closure.
Conclusion
This survey established a baseline for the community’s perceived environmental and health impacts following environmental contamination resulting from AltEn. Stress related to compromised health resulting from the situation was common among respondents. While a wide range of physical symptoms were reported, the majority were related to respiratory, allergy, or neurological (mostly headaches or migraines). Respondents were concerned about environmental contamination, primarily water, indicating access to safe and clean water as a top community need. The community also emphasized the need for proper and timely clean-up, in addition to frequent clear communication about environmental contamination and health concerns. These data can inform priorities and serve as a baseline for future health monitoring efforts. In addition, there is potential to longitudinally evaluate how community needs and perceptions of the environment change over time.
Data availability
The study data are not publicly available. Requests to access the data can be made to the corresponding author.
References
-
United States Department of Agriculture Economic Research Service. Rural Economy. Accessed November 2. 2023. https://www.ers.usda.gov/data-products/ag-and-food-statistics-charting-the-essentials/rural-economy/
-
United States Energy Information Administration. Biofuels explained Ethanol. Webpage updated 12 April 2022. Accessed November 2. 2023, and June 19, 2024. https://www.eia.gov/energyexplained/biofuels/ethanol-supply.php
-
Cimino AM, Boyles AL, Thayer KA, Perry MJ. Effects of neonicotinoid pesticide exposure on human health: A systematic review. Environ Health Perspect. 2017;125(2):155–62. https://doi.org/10.1289/EHP515
-
Douglas MR, Tooker JF. Large-Scale deployment of seed treatments has driven rapid increase in use of neonicotinoid insecticides and preemptive pest management in U.S. Field crops. Environ Sci Technol. 2015;49(8):5088–97. https://doi.org/10.1021/es506141g
-
Smith CD, Nowell LH. 2024. Health-Based Screening Levels for evaluating water-quality data (3rd ed.). U.S. Geological Survey web page, accessible at https://water.usgs.gov/water-resources/hbsl/, https://doi.org/10.5066/F71C1TWP
-
National Pesticide Information Center. EPA Pesticide Regulation. Accessed June 26. 2024. http://npic.orst.edu/reg/epareg.html
-
United States Environmental Protection Agency. Pesticide Tolerances: Clothianidin. 28 Aug 2012. Accessed June 26. 2024. https://www.regulations.gov/document/EPA-HQ-OPP-2010-0217-0044
-
Bartelt-Hunt SL, Bell JE. Surface and groundwater contamination, community and ecosystem exposures are the unintentional consequences from recycling treated seed products. Environ Sci Technol. 2021;55(9):5605–7. https://doi.org/10.1021/acs.est.1c01305
-
Neb, Rev. Stat § 66–1351 (2021). https://nebraskalegislature.gov/laws/statutes.php?statute=66-1351
-
Greenberg P, Adrian C. A primer on pollution from the AltEn plant in Mead, NE. ArcGIS StoryMaps. Published July 12, 2021. Accessed November 7, 2023. https://storymaps.arcgis.com/stories/ece1aa12927a49bfa8c7d23f2e6e082f
-
Taiba J, Rogan EG, Snow DD, Achutan C, Zahid M. Characterization of environmental levels of pesticide residues in household air and dust samples near a bioenergy plant using treated seed as feedstock. Int J Environ Res Public Health. 2023;20(21):6967. https://doi.org/10.3390/ijerph20216967
-
Zahid M, Taiba, Jabeen J, Cox K, Khan A, Uhing T, Rogan EG. Pesticide residues in adults living near a bioenergy plant with 85,000 tons of contaminated wetcake. Chemosphere. 2024;349. https://doi.org/10.1016/j.chemosphere.2023.140941
-
Gillam C. Outrage as regulators let pesticides from factory pollute US town for years. The Guardian. https://www.theguardian.com/us-news/2021/may/29/environmental-catastrophe-mead-nebraska. Published May 29, 2021. Accessed November 7, 2023.
-
Ospina M, Wong LY, Baker S, Serafim AB, Morales-Agudelo P, Calafat AM. Exposure to neonicotinoid insecticides in the U.S. General population: data from the 2015–2016 National health and nutrition examination survey. Environ Res. 2019;176:108555. https://doi.org/10.1016/j.envres.2019.108555
-
Thompson DA, Kolpin DW, Hladik ML, et al. Prevalence of neonicotinoid insecticides in paired private-well tap water and human urine samples in a region of intense agriculture overlying vulnerable aquifers in Eastern Iowa. Chemosphere. 2023;319:137904. https://doi.org/10.1016/j.chemosphere.2023.137904
-
Bradley PM, Journey CA, Romanok KM, et al. Expanded Target-Chemical analysis reveals extensive Mixed-Organic-Contaminant exposure in USA streams. Environ Sci Technol. 2017;51(9):4792–802. https://doi.org/10.1021/acs.est.7b00012
-
Berens MJ, Capel PD, Arnold WA. Neonicotinoid insecticides in surface water, groundwater, and wastewater across Land-Use gradients and potential effects. Environ Toxicol Chem. 2021;40(4):1017–33. https://doi.org/10.1002/etc.4959
-
Krupke CH, Hunt GJ, Eitzer BD, Andino G, Given K. Multiple routes of pesticide exposure for honey bees living near agricultural fields. PLoS ONE. 2012;7(1):e29268. https://doi.org/10.1371/journal.pone.0029268
-
Boyd WA, Boyles AL, Blain RB et al. NTP Research Report on the Scoping Review of Potential Human Health Effects Associated with Exposures to Neonicotinoid Pesticides: Research Report 15. National Toxicology Program; 2020. Accessed October 10, 2023. http://www.ncbi.nlm.nih.gov/books/NBK563583/
-
Zhang D, Lu S. Human exposure to neonicotinoids and the associated health risks: A review. Environ Int. 2022;163:107201. https://doi.org/10.1016/j.envint.2022.107201
-
Godbole AM, Moonie S, Coughenour C, Zhang C, Chen A, Vuong AM. Exploratory analysis of the associations between neonicotinoids and measures of adiposity among US adults: NHANES 2015–2016. Chemosphere. 2022;300:134450. https://doi.org/10.1016/j.chemosphere.2022.134450
-
Zhao H, Gui W, Tan X, Chen Y, Ning Y, Wang X. Exploratory analysis of the associations between neonicotinoids insecticides and serum lipid profiles among US adults: A cross-sectional, population-based study. Ecotoxicol Environ Saf. 2023;268:115724. https://doi.org/10.1016/j.ecoenv.2023.115724
-
Forrester MB. Neonicotinoid insecticide exposures reported to six poison centers in Texas. Hum Exp Toxicol. 2014;33(6):568–73. https://doi.org/10.1177/0960327114522500
-
Mohamed F, Gawarammana I, Robertson TA, et al. Acute human Self-Poisoning with Imidacloprid compound: A neonicotinoid insecticide. PLoS ONE. 2009;4(4):e5127. https://doi.org/10.1371/journal.pone.0005127
-
Elfman L, Hogstedt C, Engvall K, Lampa E, Lindh CH. Acute health effects on planters of conifer seedlings treated with insecticides. Ann Occup Hyg. 2009;53(4):383–90. https://doi.org/10.1093/annhyg/mep016
-
Ng AE, Boersma P. Diagnosed allergic conditions in adults: United States, 2021. NCHS Data Brief, no 460. Hyattsville, MD: National Center for Health Statistics. 2023. https://doi.org/10.15620/cdc:122809
-
Centers for Disease Control and Prevention. National Center for Health Statistics. Chronic Sinusitis. 2018. Accessed March 2025. https://www.cdc.gov/nchs/fastats/sinuses.htm
-
Burch R, Rizzoli P, Loder E. The prevalence and impact of migraine and severe headache in the united States: figures and trends from government health studies. Headache. 2018;496–505.
-
Terlizzi EP, Zablotsky B. Symptoms of anxiety and depression among adults: United States, 2019 and 2022. National Center for Health Statistics Report; no 213. Hyattsville, MD: National Center for Health Statistics. 2024. https://doi.org/10.15620/cdc/64018
-
Wu MJ, Zhao K, Fils-Aime F. Response rates of online surveys in published research: A meta-analysis. Comput Hum Behav Rep. 2022;7:100206. https://doi.org/10.1016/j.chbr.2022.100206
Acknowledgements
The authors want to thank the University of Nebraska Lincoln Bureau of Sociological Research (BOSR), specifically Amanda Ganshert for her assistance with data collection and for providing feedback related to the survey methodology. We would also like to thank Meghan Langel for logistical support.
Funding
This research was funded by the Claire M. Hubbard Foundation and by Nebraska Legislature with American Rescue Plan Act funds.
Author information
KCG data analysis, prepared tables and figures and wrote first draft and prepared the manuscript for submission. KJ data collection and provided substantial feedback on the manuscript. RM data analysis and visualization. JT project administration, survey design, reviewed and provided substantial feedback on manuscript drafts. KWK, KM, ER, PG, JEB study conception and survey design, reviewed and provided substantial feedback on manuscript drafts. ER funding acquisition. TU reviewed and provided substantial feedback on manuscript drafts. All authors read and approved the final manuscript.
Ethics declarations
This study was approved by the University of Nebraska Medical Center Institutional Review Board.
Not applicable.
The authors declare no competing interests.
Additional information
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Search
RECENT PRESS RELEASES
Related Post