Longitudinal association of community and residential environment with the risk of cogniti
April 16, 2025
Abstract
Cognitive impairment has emerged as a critical global public health issue. This study investigated the association between community and residential environments and the risk of cognitive impairment among Chinese middle-aged and older adults. The study included a final sample of 10,471 participants from the 2011–2020 The China Health and Retirement Longitudinal Study (CHARLS) cohort. Community and residential environment, and cognitive impairment, were assessed using several cognitive tests. The analyzed using the Cox Proportional Hazards Mode adjusting for age, gender, education level, marital status, residence areas, Body Mass Index (BMI), smoking status, alcohol consumption and chronic disease status. After adjusting for all Covariates, participants residing in relaxed community-based residential environments exhibited a 3.8% increased risk of cognitive impairment compared to those in crowded community environments (HR = 1.038). Middle-aged and older adults with access to garbage disposal services had a 19.3% reduced risk of cognitive impairment (HR = 0.807). Community environments featuring age-friendly facilities, such as open-air fitness equipment (HR = 0.834) and accessibility for handicapped individuals (HR = 0.948), were associated with a 16.6% and 5.2% reduction in the risk of cognitive impairment, respectively. In community social support environments, having a social organization for the older adults was associated with a 16.2% reduction in cognitive impairment risk among middle-aged and older adults (HR = 0.838). Regarding housing factors, concrete and steel buildings were associated with an 18.7% lower risk of cognitive impairment compared to adobe or other types of buildings (HR = 0.813). Domestic amenities, including running water supply (HR = 0.847), broadband connectivity (HR = 0.650), and use of clean energy (HR = 0.957), were associated with a 15.3%, 35%, and 4.3% reduction in the risk of cognitive impairment, respectively. Additionally, indoor tidiness (HR = 0.875) was associated with a 12.5% reduction in cognitive impairment risk. The good community and residential environment are correlated with the lower risk of cognitive impairment in middle-aged and older Chinese adults. Specifically, for the prevention and control of cognitive impairment, community and residential planning and construction should prioritize both the basic social and environmental factors and the internal built environment.
Introduction
Cognitive impairment has emerged as a critical global public health issue, significantly heightening the risk of adverse outcomes such as dementia and mortality1. This issue has profound implications for the health of middle-aged and older adults2,3,4. According to projections, the number of individuals with dementia worldwide is expected to reach 152Â million by 2050, leading to health care costs amounting to 1% of the global gross product annually5. Additionally, the prevalence of mild cognitive impairment among the older adults in China is 15.54%. Moreover, the number of dementia-related deaths in China rose from 1.6Â million in 1990 to 2.3Â million in 20166, presenting a significant challenge to social and economic development1. Given the absence of effective pharmacologic treatments for cognitive impairment, identifying and managing risk factors is crucial7.
Studies have shown that the community environment refers to the combination of external conditions surrounding the living spaces of community residents, encompassing multiple dimensions (e.g., infrastructure)8. In contrast, the residential environment primarily focuses on the specific places where residents live, as well as the physical and cultural conditions in their immediate surroundings9. While studies have shown that favorable residential environmental conditions exert a protective effect on cognitive function10. Greater availability of physical and social resources within a Residential community is generally associated with improved cognitive performance11,12,13. Conversely, individuals residing in less optimal environments often require increased physiological compensation14, which can accelerate biological decline and contribute to the onset of cognitive impairment and dementia15,16. Additionally, research has highlighted variations in the impact of different residential settings on cognitive function8, and community social environments may mitigate or delay cognitive decline through various physiological mechanisms17. For instance, the presence of senior activity centers can safeguard cognitive function in middle-aged and older adults by facilitating social engagement18. Moreover, enhanced physical conditions within the community, such as disability accommodations, transportation routes, and employment services, have been shown to decelerate the rate of cognitive decline19.
Although numerous studies have investigated factors influencing cognitive dysfunction20, the relationship between various dimensions of the community environment and cognitive impairment in the older adults remains unclear. Additionally, most existing research has been conducted in Western or developed countries21, with limited attention given to China, a developing country. This results in a lack of sample representativeness and necessitates further validation of the applicability of these findings to China. Moreover, many current studies are cross-sectional, which affects the overall quality of the evidence. To address these gaps, the present study examines the relationship between community environment, housing, and the incidence of cognitive dysfunction among middle-aged and older adults in China through a cohort study featuring a representative 9-year follow-up sample. The findings are intended to inform the development of relevant policies aimed at the prevention and control of cognitive impairment in China.
Methods
Research subjects
The data for this study are derived from the China Health and Retirement Longitudinal Survey (CHARLS), a project jointly initiated by several departments at Peking University. CHARLS targets middle-aged and older adults aged 45 and above in China, focusing primarily on issues related to the aging population. The baseline survey of CHARLS began in 2011 and spans 28 provinces and municipalities, including 150 county-level units, 450 village-level units, and approximately 17,000 individuals from around 10,000 households. The survey covers both urban and rural areas and is conducted every 2–3 years. The CHARLS database includes information on individual demographics, family structure, health status and functioning, physical measurements, and community characteristics, providing high-quality data for this study. The CHARLS database has been approved by the Ethical Review Committee of Peking University and all participants have signed the informed consent.
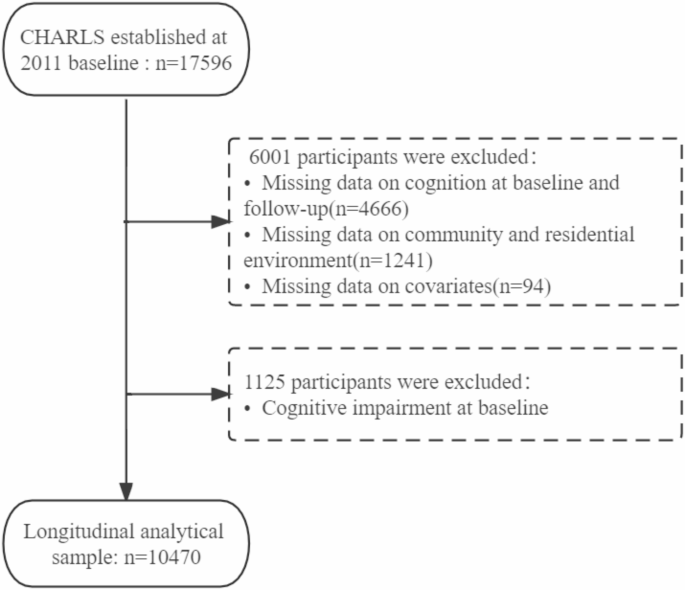
For the purpose of ensuring the reliability of the empirical analysis, data from the years 2011 to 2020 (2013, 2015, 2018 and 2020) were selected. We integrated individual information from 3 waves of data and corresponding community information based on ID matching. Data mismatches were removed, and only matched records were retained. Furthermore, we excluded records with missing data on key variables such as cognitive impairment (n = 4666), Community and Residential Environment (n = 1241), and Covariates including age, gender, and marital status (n = 94). Data that were already present from the 2011 questionnaire were also excluded. After these refinements, a total of 10,470 records with complete data on cognitive issues were included in the final analysis (Fig. 1).
Assessment indicators
Community and residential environment
Drawing from the comprehensive data on the community environment gathered through the CHARLS questionnaire, including information on roads, traffic conditions, infrastructure, convenience stores, farmers’ markets, and various other services and amenities, this study divides the analytical scope into 2 primary categories: the community environment and the residential environment (Supplement Table 1).
-
(1)
Community Environment: (a) Basic community habitat includes several aspects: “Sewerage system�, “Garbage disposal�, “Road material�, “Cleanliness of roads�, and “Relaxation of community�. For the “Sewerage System� and “Garbage Disposal�, they are each set to binary values of ‘1’ and ‘0’ to indicate their presence or absence. For “Garbage disposal�, ‘1’ signifies centralized disposal methods, while ‘0’ represents local landfill, organized incineration, dumping in rivers, or no centralized disposal. When it comes to “Road material�, asphalt/concrete roads are marked as ‘1’, whereas dirt, gravel, highway, and other types of roads are denoted as ‘0’. “Road cleanliness� and “Community relaxation� are both rated on a scale of 1 to 7, with higher numbers indicating better cleanliness or a more relaxed community environment. (b) The community facilities and environment for the older adults comprise 3 key indicators: community facilities specifically catered to the older adult’s open-air fitness equipment, and mobility accessibility for the disabled. Community living facilities for the older adults include post offices, libraries, police stations/guard rooms, banks, cinemas/theaters, convenience stores, farmers’ markets, and supermarkets. Each of these facilities, when available, is set as “1�, and when not available, as “0�. The total score for this indicator ranges from 0 to 8 points. Open-air fitness equipment is similarly marked as “1� when present and “0� when absent. The degree of accessibility for people with disabilities is rated on a 7-point scale, ranging from “no� to “very convenient�. (c) The community social support environment encompasses senior recreational organizations and senior social organizations. Senior recreational organizations, such as calligraphy and painting associations, dance teams, or other exercise teams, are marked as “1� when present and “0� when absent. Similarly, senior social organizations aimed at assisting the older adults, the sick, and the disabled, as well as senior associations, follow the same binary coding. Additionally, 2 indicators related to transportation are considered: “number of buses to villages/communities� and “distance to most frequently visited bus stops�. These indicators have values that range from 0 to 32 and 0–100 km, respectively, providing quantitative measures of the community’s social support environment.
-
(2)
Residential Environment: Residential environment encompasses 4 dimensions: external architectural features, internal spatial layout, household amenities, and indoor environment22. External architectural features include building structure type, building age (years), and building type. Building structure types are categorized as adobe, concrete and steel, brick, and wood, with each item rated on a scale of “1–3�; building age is categorized as < 10 years, 10–30 years, and > 30 years, with each item rated on a scale of “1–3�; and building type is classified as independent floor building, composite building, and multi-storey building, with each item rated on a scale of “1–2�. Internal spatial layout includes bedroom, living room, bathroom, kitchen, and balcony, with one set to “1� and others set to “0�. Household amenities include toilet type, flushable toilet, electricity supply, running water supply, natural gas supply, heating facilities, bathroom facilities, telephone connection, broadband connection, and other amenities. Household amenities are categorized as: toilet type, flushable toilet, electricity supply, mains water supply, gas supply, heating facilities, bathroom facilities, telephone connection, and broadband connection, with each item set to “1� and none set to “0�. Heating energy sources are rated on a scale from 1 to 6 (straw/wood, solar, coal, gas, electricity, other); and cooking fuel sources are categorized into 6 ratings from 1 to 6 (straw/wood, coal, natural gas, liquefied petroleum gas, electricity, other). Indoor cleanliness is rated on a scale from 1 to 5 (poor, fair, clean, very clean, excellent).
Cognitive function
This study assessed cognitive function through measures of episodic memory and executive function. episodic memory was evaluated by immediate and delayed recall tasks, where participants read a list of 10 unrelated Chinese words. The number of correctly recalled words was recorded immediately (immediate recall) and again 4 min later (delayed recall). Recalling a word correctly earns one score. The average of these immediate and delayed recall scores was calculated18, with scores ranging from 0 to 1018,23. Executive function was assessed using the Telephone Interview for Cognitive Status (TICS)24and the Figure Drawing test. TICS, a reliable and valid tool for screening cognitively impaired older adults24, includes questions about the current date (month, day, year, and season), the day of the week (with one point awarded for each successful operation), and a task to subtract 7 consecutively from 100 (one point awarded for each successful operation for a total of 5 times). In the Figure Drawing test, participants were asked to draw a picture, 1 for drawing a picture, 0 for not drawing a picture. The executive function score (range: 0–11) was derived from TICS and the Figure Drawing test, and the total cognitive function score was calculated by summing the situational memory and executive function scores, with higher scores indicating better cognitive function (range: 0–20)25. A total cognitive function score below 6 is classified as indicative of cognitive impairment26,27.
Covariates
Covariates included: (1) Individual variables: age, gender (male, female), education level (high school or below, university or higher), marital status (married, unmarried, other), and urban or rural location (main urban area, combined urban/rural area, other); (2) Health-related variables: Body Mass Index (BMI) (underweight BMI < 18.5, normal 18.5 ≤ BMI < 25, overweight 25 ≤ BMI < 30, obese BMI ≥ 30); (3) Lifestyle variables: smoking status (current smoker, former smoker, never smoked), alcohol consumption (current drinker, former drinker, never drank); (4) Chronic disease status (yes/no): including hypertension, hyperlipidemia, diabetes, and lung disease.
Statistical analysis
Descriptive statistics were utilized to evaluate the basic characteristics of the participants, with results presented as frequencies (n) and percentages (%). To examine the relationship between community and residential environment with cognitive impairment, we employed multiple Cox proportional hazards regression models. For the incidence of cognitive impairment, event time was defined as the period from the date of recruitment to the end of follow-up, or to the date of cognitive impairment diagnosis, whichever occurred first. Hazard ratios (HR) and their corresponding 95% confidence intervals (CI) were calculated and reported. To account for potential confounding effects, 3 distinct models were developed: Model 1 adjusted for age and gender; Model 2 adjusted for age, gender, smoking status, comorbidities, and alcohol consumption; and Model 3 further adjusted for place of residence, income, education, and employment status in addition to the covariates included in Model 2. All statistical analyses were conducted using STATA 14, SPSS 23, and R software, with a significance level set at a P value of less than 0.05.
Results
Characteristics of study participants
A total of 10,470 middle-aged and older adults (male: 5241; female: 5229) were included in the final statistical analysis. The mean follow-up time was 7.04 (± 2.64) years. Of these participants, 60.6% were aged between 45 and 60 years. The majority of the older adults (90.7%) were partnered. Additionally, 51.3% of the participants resided in non-urban or urban-rural combined areas. Nearly half of the study subjects (43.0%) had received an education level of elementary school or below. The prevalence of chronic illnesses was 66.9%, while 31.9% were smokers and 34.7% were alcohol drinkers (Table 1).
Relationship between community and residential environment with risk of cognitive impairment
In examining the relationship between neighborhood environmental factors and cognitive impairment, results from Model 3 indicated that participants living in neighborhoods with a relaxed community environment had a 4% increased risk of cognitive impairment (HR = 1.040, 95% CI 1.009–1.072) compared to those in more crowded environments. Conversely, neighborhoods with regular garbage disposal services were associated with a 19.3% reduction in the risk of cognitive impairment (HR = 0.807, 95% CI 0.710–0.916). In environments with age-friendly facilities, the presence of open-air fitness equipment (HR = 0.834, 95% CI 0.731–0.951) and accessible facilities for handicapped individuals (HR = 0.948, 95% CI 0.910–0.987) were associated with a 16.6% and 5.2% reduction in cognitive impairment risk, respectively. Additionally, communities with social organizations for older adults (HR = 0.838, 95% CI 0.750–0.935) significantly reduced the risk of cognitive impairment by 16.2%. Conversely, an increased distance to the nearest bus stop was associated with a 0.7% higher risk of cognitive impairment (HR = 1.007, 95% CI 1.002–1.011) (Table 2).
Regarding residential environmental factors, housing constructed from concrete and steel (HR = 0.813, 95% CI 0.774–0.838) was associated with 18.7% reduction in cognitive impairment risk compared to buildings made of adobe or other materials. Concerning home facilities, having an electricity supply (HR = 1.135, 95% CI 1.002–1.287) was linked to a 13.5% increased risk of cognitive impairment. In contrast, the presence of running water (HR = 0.847, 95% CI 0.764–0.940), bathroom facilities (HR = 0.870, 95% CI 0.771–0.981), a broadband connection (HR = 0.650, 95% CI 0.519–0.805), clean energy use (HR = 0.957, 95% CI 0.932–0.983), and heating facilities (HR = 0.957, 95% CI 0.932–0.983) were associated with reductions in cognitive impairment risk by 15.3%, 13.0%, 35.0%, 4.3%, and 4.3%, respectively. Additionally, greater indoor tidiness was associated with a 12.5% reduction in the risk of cognitive impairment (HR = 0.875, 95% CI 0.834–0.919) (Table 3).
Discussion
This study found that good community and residential environment are correlated with the lower risk of cognitive impairment. Specifically, aspects such as the basic human environment of the community (e.g., garbage disposal and road cleanliness), age-friendly facilities within the community (e.g., outdoor gyms and accessibility for the disabled), the social support environment (e.g., social organizations), concrete and steel building structures, household amenities (e.g., running water, bathroom facilities, broadband connection, heating), and the tidiness of indoor environments were all associated with a reduced risk of cognitive impairment. Conversely, factors such as community spaciousness, distance to bus stops, electricity supply, and heating facilities were found to increase the risk of cognitive impairment.
The study emphasizes that a favorable community environment is associated with a reduced risk of cognitive impairment in both middle-aged and older adults. Previous research has highlighted the significance of the community environment in shaping the daily healthy lifestyles and social interactions of older adults28,29,30, with high spatial quality being crucial for both physical and mental health31. In community-based human settlements, the lack of centralized garbage disposal will more easily lead to a reduction in the living space of urban residents, which is prone to breeding flies, mosquitoes and rats and other organisms that spread germs, affecting the cityscape and adversely affecting the physical and mental health of nearby residents, and has become one of the major environmental problems facing our country32. Therefore, effective garbage disposal and a clean, tidy community environment can enhance mood, which may explain the protective effect of proper waste management on cognitive health in the older adults. The aesthetic quality of a community is fundamental to residential comfort33, aligning with our finding that road cleanliness positively impacts cognitive function in older adults. Furthermore, the availability of community age-friendly facilities, such as open-air fitness equipment, can encourage social interaction and counteract sedentary behavior34,35, thereby benefiting cognitive function. For individuals with disabilities, supportive living environments are crucial for delaying physical decline and maintaining independence and well-being36. Compliance with the law of degradation of bodily functions, the community environment out of the positive improvement and adaptation to enhance the quality of life has an extremely important role37. Therefore, the community disabled people with high level of convenience to improve the cognitive status. Regarding the social support environment of the community, previous studies have indicated that homebound older adults who engage actively in community affairs can enhance neighborhood cohesion and a sense of belonging38,39. Greater community resources and stronger neighborhood reciprocity contribute to better mental health in older adults40, supporting our finding that social organization services can reduce the risk of cognitive impairment. Additionally, research suggests that proximity to public transportation stops can enhance mobility, promoting physical activity and improving cognitive status41. Our findings also suggest that while community spaciousness might increase the risk of cognitive impairment, this may be due to dense environments fostering more harmonious social networks and providing more opportunities for socialization42. However, further high-quality studies are needed to explore this aspect more thoroughly. In conclusion, optimizing community environments represents a promising strategy for the prevention and management of cognitive impairment in middle-aged and older adults.
Our study identified that concrete and steel structures, home amenities, and indoor environmental cleanliness in residential settings can significantly influence the risk of cognitive impairment among middle-aged and older Chinese adults. Previous research has established a connection between building type and mental health43,44,45, with a predominant focus on the quality of buildings rather than their structural type9,46. Our study, however, presents novel findings, demonstrating that concrete and steel buildings are effective in reducing the risk of cognitive impairment, which may be related to the dust-free environment of reinforced concrete buildings, while may affect the physiological aging process of the brain affecting cognition47,48. Additionally, our analysis indicates that home equipment and amenities have a significant association with cognitive impairment in older adults, aligning with existing literature49,50,51. Specifically, tap water supply services improve indoor environmental factors such as temperature and humidity50,52. The use of aluminum flocculants in tap water has been shown to lower aluminum concentration, which is linked to a reduced risk of cognitive impairment, consistent with findings that fluoridation of tap water improves cognitive functioning53. Aluminum in water has been implicated in various detrimental effects in the brain, including amyloid formation, pro-inflammatory signaling, disruption of innate immunity, neurodegeneration, and altered expression of fundamental genetic information54,55. These observations support our conclusion that tap water supply reduces the risk of cognitive impairment. Furthermore, Blay et al. reported that housing showers decrease the likelihood of headaches and mood disturbances in older adults44, contributing to a more comfortable living environment and reduced cognitive risk in middle-aged and older individuals. Our findings also indicate that broadband connectivity helps mitigate the risk of cognitive impairment in older adults, likely due to the unrestricted access to information and enhanced communication with family and friends, which alleviates loneliness56,57 and improves cognitive function58. Research on brain plasticity has shown that stimuli related to social activities can stimulate angiogenesis, synaptic formation, and neurogenesis in the brain59,60, potentially explaining the cognitive benefits associated with broadband connectivity. It is important to note that the majority of participants in this study were from rural areas (81.4%). Statistics reveal that by the end of 2016, coal-fired heating accounted for approximately 83% of the total heating area in China, with an annual consumption of around 400Â million tons of standard coal. Notably, about 50% of this was bulk-burned coal and coal used in inefficient small boilers, predominantly found in rural areas61. Data show that pollutants emitted from the direct combustion of loose coal are over 10 times greater than those from industrial coal combustion with centralized abatement62. The combustion of coal releases numerous harmful pollutants, which indirectly impact cognitive function. Particulate matter is transferred from the pulmonary system to the central nervous system via the blood-brain barrier, leading to pathophysiological changes within the central nervous system63. Moreover, air pollution has been linked to cognitive impairment through several mechanisms, including alterations in brain morphology64, damage to gray and white matter65, and the promotion of small vessel ischemic disease66. Therefore, heating facilities increase the risk of cognitive impairment in the older adults. Future research should focus on selecting appropriate heating energy sources, improving the rural energy structure, and increasing the availability of clean energy. Additionally, there have been reports of psychiatric or somatic symptoms linked to exposure to electromagnetic fields (EMFs) from electricity supply67. Exposure to electromagnetic radiation has been associated with symptoms such as poor sleep and fatigue68,69, which may explain the observed increase in cognitive dysfunction related to electricity supply. This finding necessitates further investigation through high-quality studies to confirm the effects due to the limitations of our current study.
Strengths and limitations
The strengths of our study lie in its high-quality cohort design with a nine-year follow-up period, ensuring reliability. The sample’s representativeness allows for generalizations to the broader Chinese population. Additionally, we have carefully considered and adjusted for nine covariates, enhancing the study’s rigor. However, there are limitations, primarily related to the self-reporting of indicators, which may introduce bias, where changes in test variables over time could lead to errors. Additionally, studies with larger sample sizes are more likely to detect significant effects compared to those with smaller samples, which increases the potential for Type I errors. Another limitation is the accuracy of the determination of cognitive impairment, which may not be precise enough and could impact the results to some extent. Furthermore, incomplete control of certain variables may introduce biases into the findings. Lastly, the use of simple Cox regression models in this study does not fully account for inter-individual and inter-regional dependencies, and future studies could consider using multi-level models to better address these complexities.
Conclusion
Our study highlights the significant role of community and residential environments in reducing the risk of cognitive impairment among middle-aged and older adults. Specifically, we identified several factors, including socially based human environments, age-friendly community facilities, social support environments, building structures, home amenities, and indoor environmental cleanliness, that contribute to this risk reduction. Conversely, factors such as community spaciousness, distance to bus stops, electricity supply, and heating facilities are associated with an increased risk. In addition, the most critical influencing factors are garbage disposal in community basic living environment and internet connection in household facilities and indoor environment. These findings have important implications for the development of policies and strategies aimed at enhancing cognitive health in this population through modifications to their community and residential environments.
Data availability
Data used for this study are available on the CHARLS website: https://charls.pku.edu.cn/.
Abbreviations
- HR:
-
Hazard ratios
- CI:
-
Confidence intervals
- CHARLS:
-
China health and retirement longitudinal study
- EMFs:
-
Exposure to electromagnetic fields
- BMI:
-
Body Mass Index
6. References
-
Phelan, E. A. et al. Association of incident dementia with hospitalizations. JAMA 307 (2), 165–172 (2012).
-
Langa, K. M. et al. Trends in the prevalence and mortality of cognitive impairment in the united States: Is there evidence of a compression of cognitive morbidity? Alzheimers Dement. 4 (2), 134–144 (2008).
-
Hao, Q. et al. Frailty and cognitive impairment in predicting mortality among Oldest-Old people. Front. Aging Neurosci. 10, 295 (2018).
-
Perna, L. et al. Cognitive impairment, all-cause and cause-specific mortality among non-demented older adults. Age Ageing. 44 (3), 445–451 (2015).
-
Kivipelto, M., Mangialasche, F. & Ngandu, T. Lifestyle interventions to prevent cognitive impairment, dementia and alzheimer disease. Nat. Rev. Neurol. 14 (11), 653–666 (2018).
-
Jia, J. et al. The prevalence of mild cognitive impairment and its etiological subtypes in elderly Chinese. Alzheimers Dement. 10 (4), 439–447 (2014).
-
Sun, W. L. et al. Research progress on risk prediction models of cognitive impairment in the elderly. (Chinese Nursing Management, 2022).
-
Putrik, P. et al. Living environment matters: Relationships between neighborhood characteristics and health of the residents in a Dutch municipality. J. Community Health. 40 (1), 47–56 (2015).
-
Howden-Chapman, P. L. et al. The effect of housing on the mental health of older people: The impact of lifetime housing history in Whitehall II. BMC Public Health. 11, 682 (2011).
-
Hou, F. The Study of the Correlation between Living Environment, Built Environment and Mild Cognitive Impairment among Older Adults 56 (China National Knowledge Infrastructure, 2023).
-
Lanza, S. T., Coffman, D. L. & Xu, S. Causal inference in latent class analysis. Struct. Equ Model. 20 (3), 361–383 (2013).
-
Szreter, S. & Woolcock, M. Health by association? Social capital, social theory, and the political economy of public health. Int. J. Epidemiol. 33 (4), 650–667 (2004).
-
Lai, K. Y. et al. Neighbourhood residential density, urbanicity and incident dementia and Alzheimer’s disease: A 12-year prospective cohort study from the UK biobank. Environ. Res. 226, 115627 (2023).
-
Cawthon, R. M. et al. Association between telomere length in blood and mortality in people aged 60 years or older. Lancet 361 (9355), 393–395 (2003).
-
Simons, R. L. et al. The effects of social adversity, discrimination, and health risk behaviors on the accelerated aging of African Americans: Further support for the weathering hypothesis. Soc. Sci. Med. 282, 113169 (2021).
-
Ouanes, S. & Popp, J. High cortisol and the risk of dementia and Alzheimer’s disease: A review of the literature. Front. Aging Neurosci. 11, 43 (2019).
-
Glei, D. A. et al. Participating in social activities helps preserve cognitive function: An analysis of a longitudinal, population-based study of the elderly. Int. J. Epidemiol. 34 (4), 864–871 (2005).
-
Lei, X. et al. Gender differences in cognition among older adults in China. J. Hum. Resour. 47 (4), 951–971 (2012).
-
Luo, Y., Zhang, L. & Pan, X. Neighborhood environments and cognitive decline among Middle-Aged and older people in China. J. Gerontol. B Psychol. Sci. Soc. Sci. 74 (7), e60–e71 (2019).
-
Evans, G. W. The built environment and mental health. J. Urban Health. 80 (4), 536–555 (2003).
-
Zheng, G. L. S. W. Urban-Rural Differences in the Effect of Community Poverty on Elderly Mental Health——A Study Based on the 2014 Chinese Longitudinal Aging Social Survey (Population and Development, 2019).
-
Firdaus, G. Built Environment and Health Outcomes: Identification of Contextual Risk Factors for Mental Well-being of Older Adults. (2017).
-
McArdle, J. J., Fisher, G. G. & Kadlec, K. M. Latent variable analyses of age trends of cognition in the health and retirement study, 1992–2004. Psychol. Aging. 22 (3), 525–545 (2007).
-
Seo, E. H. et al. Validity of the telephone interview for cognitive status (TICS) and modified TICS (TICSm) for mild cognitive imparment (MCI) and dementia screening. Arch. Gerontol. Geriatr. 52 (1), e26–30 (2011).
-
Chen, C. et al. Cognitive frailty in relation to adverse health outcomes independent of Multimorbidity: Results from the China health and retirement longitudinal study. Aging (Albany NY). 12 (22), 23129–23145 (2020).
-
Jak, A. J. et al. Quantification of five neuropsychological approaches to defining mild cognitive impairment. Am. J. Geriatr. Psychiatry. 17 (5), 368–375 (2009).
-
Li, C. et al. Catastrophic health expenditure among Chinese adults living alone with cognitive impairment: Findings from the CHARLS. BMC Geriatr. 22 (1), 640 (2022).
-
Thorsson, S., Lindqvist, M. & Lindqvist, S. Thermal bioclimatic conditions and patterns of behaviour in an urban park in Goteborg, Sweden. Int. J. Biometeorol. 48 (3), 149–156 (2004).
-
Spagnolo, J. & De Dear, R. A field study of thermal comfort in outdoor and semi – outdoor environments in subtropical Sydney Australia. Build. Environ. (2003).
-
Kim, H. & Macdonald, E. Measuring the effectiveness of san francisco’s planning standard for pedestrian wind comfort. Int. J. Sustain. Dev. World Ecol. (2017).
-
Burton, E. J., Mitchell, L. & Stride, C. B. Good places for ageing in place: Development of objective built environment measures for investigating links with older People’s wellbeing. BMC Public Health. 11, 839 (2011).
-
Songao, Y. Research on the Effect of Community Elderly Facilities and Services on the Depression of Middle-aged and Elderly People. (CNKI) (2021).
-
Li Jianxin, Z. Y. The Level of Incompetence and Mental Health of the elderly: Age Differences and the Regulatory Role of Community Resources (Academia Bimestris, 2018).
-
Sugiyama, T. et al. Associations of neighbourhood greenness with physical and mental health: Do walking, social coherence and local social interaction explain the relationships? J. Epidemiol. Community Health. 62 (5), e9 (2008).
-
Sarkar, C. & Webster, C. Healthy cities of tomorrow: The case for large scale built environment-health studies. J. Urban Health. 94 (1), 4–19 (2017).
-
Shin, C. N., Lee, Y. S. & Belyea, M. Physical activity, benefits, and barriers across the aging continuum. Appl. Nurs. Res. 44, 107–112 (2018).
-
WahlH, W. H.R.W.P.G., Aging in Context: Socio-Physical Environment. (Annual view of Gerontology & Geriatrics, 2003).
-
Cramm, J. M. & Nieboer, A. P. Social cohesion and belonging predict the well-being of community-dwelling older people. BMC Geriatr. 15, 30 (2015).
-
Elliott, J. et al. Neighbourhood cohesion and mental wellbeing among older adults: A mixed methods approach. Soc. Sci. Med. 107, 44–51 (2014).
-
Alexopoulos, G. S. Depression in the elderly. Lancet 365 (9475), 1961–1970 (2005).
-
Cerin, E. et al. From urban neighbourhood environments to cognitive health: A cross-sectional analysis of the role of physical activity and sedentary behaviours. BMC Public Health. 21 (1), 2320 (2021).
-
Stahl, S. T. et al. Living alone and depression: The modifying role of the perceived neighborhood environment. Aging Ment. Health. 21 (10), 1065–1071 (2017).
-
Liu, Y. et al. Healthy urban living: Residential environment and health of older adults in Shanghai. Health Place. 47, 80–89 (2017).
-
Blay, S. L., Schulz, A. J. & Mentz, G. The relationship of built environment to health-Related behaviors and health outcomes in elderly community residents in a middle income country. J. Public Health Res. 4 (2), 548 (2015).
-
Firdaus, G. Built Environment and Health Outcomes: Identification of Contextual Risk Factors for Mental well-being of Older Adults (Ageing International, 2017).
-
Ochodo, C. et al. External built residential environment characteristics that affect mental health of adults. J. Urban Health. 91 (5), 908–927 (2014).
-
Nußbaum, R. et al. Associations of air pollution and noise with local brain structure in a cohort of older adults. Environ. Health Perspect. 128 (6), 67012 (2020).
-
Fangfang, H. et al. Living environment, built environment and cognitive function among older Chinese adults: Results from a Cross-Sectional study. J. Prev. Alzheimers Dis. 9 (1), 126–135 (2022).
-
Galea, S. et al. Urban built environment and depression: A multilevel analysis. J. Epidemiol. Community Health. 59 (10), 822–827 (2005).
-
Phillips, D. R. et al. The impacts of dwelling conditions on older persons’ psychological well-being in Hong Kong: The mediating role of residential satisfaction. Soc. Sci. Med. 60 (12), 2785–2797 (2005).
-
Xiao, Y. et al. Exploring the impacts of housing condition on migrants’ mental health in Nanxiang, Shanghai: A structural equation modelling approach. Int. J. Environ. Res. Public Health, 15(2), 225 (2018).
-
Guite, H. F., Clark, C. & Ackrill, G. The impact of the physical and urban environment on mental well-being. Public Health. 120 (12), 1117–1126 (2006).
-
Zhai, D. et al. The effect of water source on cognitive functioning in Chinese adults: A cross-sectional and follow-up study. Ecotoxicol. Environ. Saf. 230, 113156 (2022).
-
Garza-Lombó, C. et al. Neurotoxicity linked to dysfunctional metal ion homeostasis and xenobiotic metal exposure: Redox signaling and oxidative stress. Antioxid. Redox Signal. 28 (18), 1669–1703 (2018).
-
Walton, J. R. Chronic aluminum intake causes Alzheimer’s disease: Applying Sir Austin Bradford Hill’s causality criteria. J. Alzheimers Dis. 40 (4), 765–838 (2014).
-
Chou, W. H., Lai, Y. T. & Liu, K. H. User requirements of social media for the elderly: A case study in Taiwan. Behav. Inform. Technol. 32 (9), 920–937 (2013).
-
Gu, X. Mechanistic Studies of the Effects of Internet Use on Mental Health in Older People—Empirical Analysis Based on the CGSS (2021) Data (Operations Research and Fuzziology, 2023).
-
De Santis, K. K. et al. Digital technologies for health promotion and disease prevention in older people: Scoping review. J. Med. Internet Res. 25, e43542 (2023).
-
Churchill, J. D. et al. Exercise, experience and the aging brain. Neurobiol. Aging. 23 (5), 941–955 (2002).
-
Fillit, H. M. et al. Achieving and maintaining cognitive vitality with aging. Mayo Clin. Proc. 77 (7), 681–696 (2002).
-
Ziqi, Z. Study on Financial Subsidy Policy for Clean Heating in Rural Areas of Northern China. (2019) (CNKI).
-
Xie, K. Green transformation of the Wujin industry. (2016).
-
You, R., Ho, Y. S. & Chang, R. C. The pathogenic effects of particulate matter on neurodegeneration: A review. J. Biomed. Sci. 29 (1), 15 (2022).
-
Crous-Bou, M. et al. Impact of urban environmental exposures on cognitive performance and brain structure of healthy individuals at risk for Alzheimer’s dementia. Environ. Int. 138, 105546 (2020).
-
Liu, Q. et al. Air pollution particulate matter exposure and chronic cerebral hypoperfusion and measures of white matter injury in a murine model. Environ. Health Perspect. 129 (8), 87006 (2021).
-
Lecordier, S. et al. Neurovascular alterations in vascular dementia: Emphasis on risk factors. Front. Aging Neurosci. 13, 727590 (2021).
-
Szemerszky, R. et al. Polluted places or polluted Minds? An experimental sham-exposure study on background psychological factors of symptom formation in ‘idiophatic environmental intolerance attributed to electromagnetic fields’. Int. J. Hyg. Environ. Health. 213 (5), 387–394 (2010).
-
Bolte, J. F. et al. Everyday exposure to power frequency magnetic fields and associations with non-specific physical symptoms. Environ. Pollut. 196, 224–229 (2015).
-
Mortazavi, S. M. Subjective symptoms related to GSM radiation from mobile phone base stations: A cross-sectional study. J. Biomed. Phys. Eng. 4 (1), 39–40 (2014).
Acknowledgements
This research has been conducted using the CHARLS. We thank the participants of the CHARLS.
Funding
None.
Author information
Authors and Affiliations
Contributions
Writing manuscript: YZ; data extraction and statistical analysis: YZ and LM; conceptualization, project administration, and supervision: JZ. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The CHARLS database has been approved by the Ethical Review Committee of Peking University and all participants have signed the informed consent.
Consent for publication
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhang, Y., Ma, L. & Zhao, J. Longitudinal association of community and residential environment with the risk of cognitive impairment in middle-aged and older Chinese adults.
Sci Rep 15, 13233 (2025). https://doi.org/10.1038/s41598-025-97512-3
-
Received: 06 November 2024
-
Accepted: 04 April 2025
-
Published: 17 April 2025
-
DOI: https://doi.org/10.1038/s41598-025-97512-3
Keywords
Search
RECENT PRESS RELEASES
Related Post