Reducing artificial light at night exposure in the urban environment could decrease light
October 3, 2025
Abstract
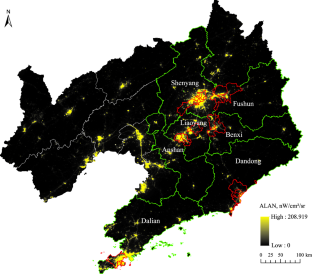
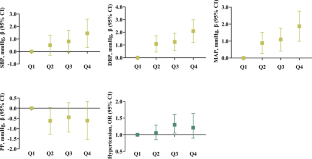
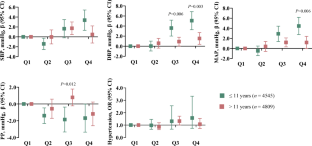
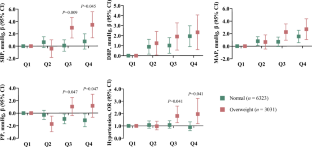
Elevated blood pressure in children is related to the hypertension in adults. Reducing environmental factors linked to hypertension in children is necessary to prevent hypertension in adults. To investigate the associations between outdoor artificial light at night (ALAN) and blood pressure among children. We recruited 9354 children aged 5–17 in the Seven Northeastern Cities Study between 2012 and 2013. Trained nurses measured their blood pressure with a mercury sphygmomanometer. We defined hypertension as systolic blood pressure (SBP) or diastolic blood pressure (DBP) ≥95th age-sex-height-specific percentile. We geocoded the address of each child and linked it to estimated outdoor ALAN within 500 m (ALAN−500 m) sourced from the VIIRS/DNB. We utilized generalized linear mixed-effect models to assess the associations of outdoor ALAN and blood pressure and the odds of hypertension. Effect modification by age, sex, weight status, and other potential factors was also explored. The SBP, DBP, and mean arterial pressure at quartile 4 (Q4) of outdoor ALAN−500 m against Q1 increased in 1.45 (95% CI: 0.31–2.59) mmHg, 2.09 (95% CI: 1.18–2.99) mmHg, and 1.87 (95% CI: 0.99–2.76) mmHg, respectively. The odds of hypertension increased by 30% in Q3 of outdoor ALAN−500 m compared to Q1 (OR = 1.30, 95% CI: 1.05–1.61). Furthermore, stronger effect estimates were observed among children aged ≤11 years (Q4, β = 5.07[3.28–6.85] vs β = 1.54[0.37–2.71] for DBP) and who were overweight (Q4, OR = 1.95[1.17–3.22] vs OR = 0.89[0.60–1.32] for hypertension). Living in areas with high outdoor ALAN exposure increased the odds of hypertension in children, especially in children aged ≤11 years and overweight. Reducing outdoor ALAN is important for preventing hypertension and controlling blood pressure in children.
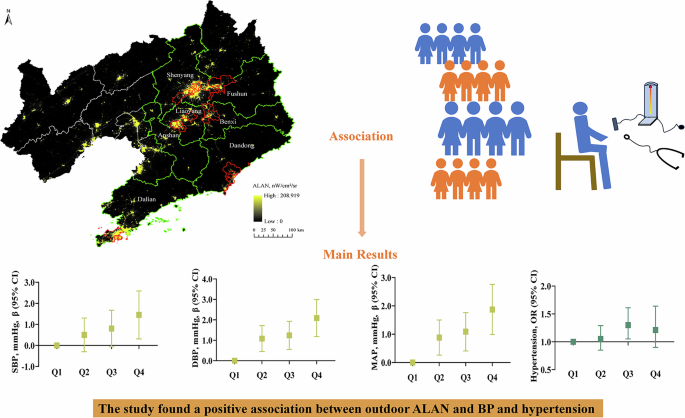
The study found a positive association between outdoor ALAN and blood pressure and hypertension
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
References
-
Fujiwara T, Kaneko H, Hayashi K, Azegami T, Mizuno A, Yano Y. Hypertension in children and adolescents: perspectives in Japan. Hypertens Res. 2024;47:3372–9.
-
Moyer VA. Screening for primary hypertension in children and adolescents: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2013;159:613–9.
-
Chen L, Zhang Y, Ma T, Liu JY, Shi D, Zhong PL, et al. [Prevalence trend of high normal blood pressure and elevated blood pressure in Chinese Han children and adolescents aged 7-17 years from 2010 to 2019]. Zhonghua Yu Fang Yi Xue Za Zhi. 2023;57:49–57.
-
Chen X, Wang Y. Tracking of blood pressure from childhood to adulthood. Circulation. 2008;117:3171–80.
-
Erlingsdottir A, Indridason OS, Thorvaldsson O, Edvardsson VO. Blood pressure in children and target-organ damage later in life. Pediatr Nephrol. 2010;25:323–8.
-
Zielinska-Dabkowska KM, Schernhammer ES, Hanifin JP, Brainard GC. Reducing nighttime light exposure in the urban environment to benefit human health and society. Science. 2023;380:1130–5.
-
Kyba CCM, Altintas YO, Walker CE, Newhouse M. Citizen scientists report global rapid reductions in the visibility of stars from 2011 to 2022. Science. 2023;379:265–8.
-
Allada R, Bass J. Circadian mechanisms in medicine. N Engl J Med. 2021;384:550–61.
-
Roenneberg T, Merrow M. The circadian clock and human health. Curr Biol. 2016;26:R432–43.
-
Crnko S, Du Pre BC, Sluijter JPG, Van Laake LW. Circadian rhythms and the molecular clock in cardiovascular biology and disease. Nat Rev Cardiol. 2019;16:437–47.
-
Steffens S, Winter C, Schloss MJ, Hidalgo A, Weber C, Soehnlein O. Circadian control of inflammatory processes in atherosclerosis and its complications. Arterioscler Thromb Vasc Biol. 2017;37:1022–8.
-
Higuchi S, Nagafuchi Y, Lee SI, Harada T. Influence of light at night on melatonin suppression in children. J Clin Endocrinol Metab. 2014;99:3298–303.
-
Chellappa SL. Individual differences in light sensitivity affect sleep and circadian rhythms. Sleep. 2021;44:zsaa214.
-
Zhang X, Zheng R, Xin Z, Zhao Z, Li M, Wang T, et al. Sex- and age-specific association between outdoor light at night and obesity in Chinese adults: a national cross-sectional study of 98,658 participants from 162 study sites. Front Endocrinol. 2023;14:1119658.
-
Shen M, Li Y, Li S, Chen X, Zou B, Lu Y. Association of exposure to artificial light at night during adolescence with blood pressure in early adulthood. Chronobiol Int. 2023;40:1419–26.
-
Sun S, Cao W, Ge Y, Ran J, Sun F, Zeng Q, et al. Outdoor light at night and risk of coronary heart disease among older adults: a prospective cohort study. Eur Heart J. 2021;42:822–30.
-
Lin LZ, Zeng XW, Deb B, Tabet M, Xu SL, Wu QZ, et al. Outdoor light at night, overweight, and obesity in school-aged children and adolescents. Environ Pollut. 2022;305:119306.
-
Paksarian D, Rudolph KE, Stapp EK, Dunster GP, He J, Mennitt D, et al. Association of outdoor artificial light at night with mental disorders and sleep patterns among U.S. adolescents. JAMA Psychiatry. 2020;77:1266–75.
-
Wang LB, Gong YC, Fang QL, Cui XX, Dharmage SC, Jalaludin B, et al. Association between exposure to outdoor artificial light at night and sleep disorders among children in China. JAMA Netw Open. 2022;5:e2213247.
-
Lane KJ, Stokes EC, Seto KC, Thanikachalam S, Thanikachalam M, Bell ML. Associations between greenness, impervious surface area, and nighttime lights on biomarkers of vascular aging in Chennai, India. Environ Health Perspect. 2017;125:087003.
-
Sorensen TB, Wilson R, Gregson J, Shankar B, Dangour AD, Kinra S. Is night-time light intensity associated with cardiovascular disease risk factors among adults in early-stage urbanisation in South India? A cross-sectional study of the Andhra Pradesh Children and Parents Study. BMJ Open. 2020;10:e036213.
-
Wang R, Hu X, Ou Y, Chen G, Wang L, Qian Z, et al. Association between outdoor light at night and hypertension and high-normal blood pressure: a nationwide cross-sectional study among Chinese adults. J Clin Hypertens. 2024;26:134–44.
-
Jacobs DR Jr., Woo JG, Sinaiko AR, Daniels SR, Ikonen J, Juonala M, et al. Childhood cardiovascular risk factors and adult cardiovascular events. N Engl J Med. 2022;386:1877–88.
-
Chung J, Robinson CH, Yu A, Bamhraz AA, Ewusie JE, Sanger S, et al. Risk of target organ damage in children with primary ambulatory hypertension: a systematic review and meta-analysis. Hypertension. 2023;80:1183–96.
-
Dong G-H, Wang J, Zeng X-W, Chen L, Qin X-D, Zhou Y, et al. Interactions between air pollution and obesity on blood pressure and hypertension in Chinese children. Epidemiology. 2015;26:740–7.
-
National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114:555–76.
-
Elvidge CD, Baugh KE, Zhizhin M, Hsu F-C. Why VIIRS data are superior to DMSP for mapping nighttime lights. Proc Asia-Pac Adv Netw. 2013;35:62–9.
-
Kyba C, Garz S, Kuechly H, de Miguel A, Zamorano J, Fischer J, et al. High-resolution imagery of Earth at night: new sources, opportunities and challenges. Remote Sens. 2014;7:1–23.
-
Elvidge CD, Baugh K, Zhizhin M, Hsu FC, Ghosh T. VIIRS night-time lights. Int J Remote Sens. 2017;38:5860–79.
-
Vollmer C, Michel U, Randler C. Outdoor light at night (LAN) is correlated with eveningness in adolescents. Chronobiol Int. 2012;29:502–8.
-
Koo YS, Song JY, Joo EY, Lee HJ, Lee E, Lee SK, et al. Outdoor artificial light at night, obesity, and sleep health: cross-sectional analysis in the KoGES study. Chronobiol Int. 2016;33:301–14.
-
Xiao Q, Gee G, Jones RR, Jia P, James P, Hale L. Cross-sectional association between outdoor artificial light at night and sleep duration in middle-to-older aged adults: the NIH-AARP diet and health study. Environ Res. 2020;180:108823.
-
Xiao X, Yang BY, Hu LW, Markevych I, Bloom MS, Dharmage SC, et al. Greenness around schools associated with lower risk of hypertension among children: findings from the seven Northeastern cities study in China. Environ Pollut. 2020;256:113422.
-
Gabinet NM, Portnov BA. Assessing the impacts of ALAN and noise proxies on sleep duration and quality: evidence from a nation-wide survey in Israel. Chronobiol Int. 2021;38:638–58.
-
Banderali G, Martelli A, Landi M, Moretti F, Betti F, Radaelli G, et al. Short and long term health effects of parental tobacco smoking during pregnancy and lactation: a descriptive review. J Transl Med. 2015;13:327.
-
Rameez RM, Sadana D, Kaur S, Ahmed T, Patel J, Khan MS, et al. Association of maternal lactation with diabetes and hypertension: a systematic review and meta-analysis. JAMA Netw Open. 2019;2:e1913401.
-
Kooiman J, Terstappen F, van Wagensveld L, Franx A, Wever KE, Roseboom TJ, et al. Conflicting effects of fetal growth restriction on blood pressure between human and rat offspring: a meta-analysis. Hypertension. 2020;75:806–18.
-
Lewandowski AJ, Levy PT, Bates ML, McNamara PJ, Nuyt AM, Goss KN. Impact of the vulnerable preterm heart and circulation on adult cardiovascular disease risk. Hypertension. 2020;76:1028–37.
-
Sorof J, Daniels S. Obesity hypertension in children: a problem of epidemic proportions. Hypertension. 2002;40:441–7.
-
Yang BY, Qian ZM, Li S, Chen G, Bloom MS, Elliott M, et al. Ambient air pollution in relation to diabetes and glucose-homoeostasis markers in China: a cross-sectional study with findings from the 33 communities Chinese Health Study. Lancet Planet Health. 2018;2:e64–73.
-
Chen G, Knibbs LD, Zhang W, Li S, Cao W, Guo J, et al. Estimating spatiotemporal distribution of PM(1) concentrations in China with satellite remote sensing, meteorology, and land use information. Environ Pollut. 2018;233:1086–94.
-
Di Q, Dai L, Wang Y, Zanobetti A, Choirat C, Schwartz JD, et al. Association of short-term exposure to air pollution with mortality in older adults. JAMA. 2017;318:2446–56.
-
Li S, Guo Y, Williams G. Acute impact of hourly ambient air pollution on preterm birth. Environ Health Perspect. 2016;124:1623–9.
-
Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Ser B Stat Methodol. 1995;57:289–300.
-
Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, Daniels SR, et al. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics. 2017;140:e20171904.
-
Huo JK, Zhou LJ, Wen B, Wang XJ, Dong B, Ma J. The method of blood pressure evaluation among children and adolescents aged 7 to 17 years old in China. Zhonghua Yu Fang Yi Xue Za Zhi. 2019;53:1299–304.
-
Curtis AM, Cheng Y, Kapoor S, Reilly D, Price TS, FitzGerald GA. Circadian variation of blood pressure and the vascular response to asynchronous stress. Proc Natl Acad Sci USA. 2007;104:3450–5.
-
Cvikova D, Sutovska H, Babarikova K, Molcan L. Hypotensive effects of melatonin in rats: focus on the model, measurement, application, and main mechanisms. Hypertens Res. 2022;45:1929–44.
-
Arangino S, Cagnacci A, Angiolucci M, Vacca AM, Longu G, Volpe A, et al. Effects of melatonin on vascular reactivity, catecholamine levels, and blood pressure in healthy men. Am J Cardiol. 1999;83:1417–9.
-
Grimaldi D, Carter JR, Van Cauter E, Leproult R. Adverse impact of sleep restriction and circadian misalignment on autonomic function in healthy young adults. Hypertension. 2016;68:243–50.
-
Hu K, Li W, Zhang Y, Chen H, Bai C, Yang Z, et al. Association between outdoor artificial light at night and sleep duration among older adults in China: a cross-sectional study. Environ Res. 2022;212:113343.
-
Zhang D, Jones RR, Powell-Wiley TM, Jia P, James P, Xiao Q. A large prospective investigation of outdoor light at night and obesity in the NIH-AARP diet and health study. Environ Health. 2020;19:74.
-
Xu YJ, Xie ZY, Gong YC, Wang LB, Xie YY, Lin LZ, et al. The association between outdoor light at night exposure and adult obesity in Northeastern China. Int J Environ Health Res. 2023;34:708–18.
-
Ai S, Li Z, Wang S, Chen S, Chan JW, Au CT, et al. Blood pressure and childhood obstructive sleep apnea: a systematic review and meta-analysis. Sleep Med Rev. 2022;65:101663.
-
Tobaldini E, Fiorelli EM, Solbiati M, Costantino G, Nobili L, Montano N. Short sleep duration and cardiometabolic risk: from pathophysiology to clinical evidence. Nat Rev Cardiol. 2019;16:213–24.
-
Jayedi A, Rashidy-Pour A, Khorshidi M, Shab-Bidar S. Body mass index, abdominal adiposity, weight gain and risk of developing hypertension: a systematic review and dose-response meta-analysis of more than 2.3 million participants. Obes Rev. 2018;19:654–67.
-
Munzel T, Sorensen M, Gori T, Schmidt FP, Rao X, Brook FR, et al. Environmental stressors and cardio-metabolic disease: part II-mechanistic insights. Eur Heart J. 2017;38:557–64.
-
Munzel T, Hahad O, Sorensen M, Lelieveld J, Duerr GD, Nieuwenhuijsen M, et al. Environmental risk factors and cardiovascular diseases: a comprehensive expert review. Cardiovasc Res. 2022;118:2880–902.
-
Cui Y, Zhang F, Wang H, Wu J, Zhang D, Xing Y, et al. Children who appeared or remained overweight or obese predict a higher follow-up blood pressure and higher risk of hypertension: a 6-year longitudinal study in Yantai, China. Hypertens Res. 2023;46:1840–9.
-
Prajapati N, Praud D, Perrin C, Fervers B, Coudon T, Faure E, et al. Outdoor exposure to artificial light at night and breast cancer risk: a case-control study nested in the E3N-generations cohort. Environ Health Perspect. 2025;133:57015.
Acknowledgements
We are very grateful to the teachers, participants, and participants’ parents or guardians from the Seven Northeastern Cities Study. We are grateful to Dr. Muhammad Amjad for revising the language in the full text.
Funding
This work was supported by the National Key Research and Development Program of China (2022YFC3702702, 2023YFC3709203), National Natural Science Foundation of China (82373536, 81872583, 82003418, 82073502), Guangxi Key Research and Development Plan (2023AB22092), Zhongnanshan Medical Foundation of Guangdong Province (ZNSXS-20230012), Scientific and Technological Projects of Shenzhen (JCYJ20230807153259001), Open Project of State Key Laboratory of Respiratory Disease (SKLRD-OP-202402). Li-Wen Hu is supported by China Scholarship Council (202106385026).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, LB., Zou, HX., Liu, XY. et al. Reducing artificial light at night exposure in the urban environment could decrease light pollution-related hypertension in children.
Hypertens Res (2025). https://doi.org/10.1038/s41440-025-02380-z
-
Received: 06 February 2025
-
Revised: 04 September 2025
-
Accepted: 15 September 2025
-
Published: 03 October 2025
-
DOI: https://doi.org/10.1038/s41440-025-02380-z
Keywords
Search
RECENT PRESS RELEASES
Related Post