The environmental exposome in heart failure risk and progression
January 25, 2026
Abstract
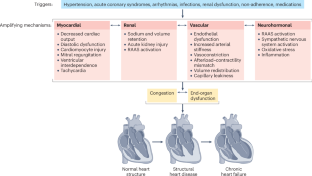
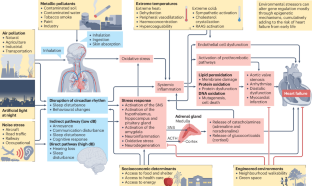
Environmental exposures have a crucial role in the incidence and progression of heart failure (HF) by exacerbating genetic predisposition and other pathophysiological mechanisms. The exposome — encompassing pollution, climate and the urban environment — and the biological responses to these factors shape cardiovascular health in complex ways. Air, noise and light pollution, exposure to toxic metals, and extremes of temperature adversely affect HF outcomes. Social determinants of health, including socioeconomic status, amplify these environmental risks, disproportionately affecting vulnerable populations. Conversely, green spaces and walkable neighbourhoods are linked to a reduced risk of HF, improved vascular health and medication adherence. Emerging evidence suggests that environmental stressors influence HF outcomes from early life by altering gene expression through epigenetic mechanisms. Despite these insights, research gaps remain. Future studies must integrate environmental, genetic and multiomics data to refine risk prediction and guide targeted public health interventions. A comprehensive understanding of the exposome in the aetiology of HF is essential for developing prevention strategies that address both biological and social determinants of cardiovascular health.
Key points
-
The environmental exposome encompasses the cumulative effects of external and internal factors influencing the risk and progression of heart failure (HF).
-
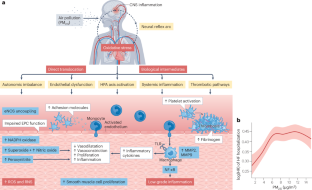
Air pollution, particularly particulate matter with an aerodynamic diameter <2.5 µm, significantly elevates the risk of HF through inflammatory and oxidative pathways.
-
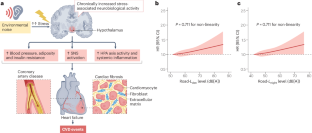
Chronic noise exposure disrupts autonomic balance, increasing the risk of HF and adverse cardiovascular events.
-
Toxic metals, such as cadmium and lead, exacerbate oxidative stress, contributing to myocardial damage and the progression of HF.
-
Climate conditions, artificial light and socioeconomic disparities further compound the risk of HF, necessitating comprehensive public health interventions.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 /Â 30Â days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$189.00 per year
only $15.75 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

References
-
Ran, J. et al. Global, regional, and national burden of heart failure and its underlying causes, 1990–2021: results from the global burden of disease study 2021. Biomark. Res. 13, 16 (2025).
-
Al-Kindi, S. G., Brook, R. D., Biswal, S. & Rajagopalan, S. Environmental determinants of cardiovascular disease: lessons learned from air pollution. Nat. Rev. Cardiol. 17, 656–672 (2020).
-
Chatterjee, N., Gim, J. & Choi, J. Epigenetic profiling to environmental stressors in model and non-model organisms: ecotoxicology perspective. Environ. Health Toxicol. 33, e2018015 (2018).
-
Hala, D., Huggett, D. & Burggren, W. Environmental stressors and the epigenome. Drug Discov. Today Technol. 12, e3–e8 (2014).
-
Perera, F. & Herbstman, J. Prenatal environmental exposures, epigenetics, and disease. Reprod. Toxicol. 31, 363–373 (2011).
-
Wild, C. P. Complementing the genome with an “exposome�: the outstanding challenge of environmental exposure measurement in molecular epidemiology. Cancer Epidemiol. Biomarkers Prev. 14, 1847–1850 (2005).
-
Daiber, A. et al. The “exposome� concept — how environmental risk factors influence cardiovascular health. Acta Biochim. Pol. 66, 269–283 (2019).
-
Münzel, T., Sørensen, M., Hahad, O., Nieuwenhuijsen, M. & Daiber, A. The contribution of the exposome to the burden of cardiovascular disease. Nat. Rev. Cardiol. 20, 651–669 (2023).
-
Khraishah, H., Chen, Z. & Rajagopalan, S. Understanding the cardiovascular and metabolic health effects of air pollution in the context of cumulative exposomic impacts. Circ. Res. 134, 1083–1097 (2024).
-
Rajagopalan, S., Al-Kindi, S. G. & Brook, R. D. Air pollution and cardiovascular disease: JACC state-of-the-art review. J. Am. Coll. Cardiol. 72, 2054–2070 (2018).
-
Khraishah, H. et al. Climate change and cardiovascular disease: implications for global health. Nat. Rev. Cardiol. 19, 798–812 (2022).
-
Münzel, T. et al. Environmental noise and the cardiovascular system. J. Am. Coll. Cardiol. 71, 688–697 (2018).
-
Zielinska-Dabkowska, K. M., Schernhammer, E. S., Hanifin, J. P. & Brainard, G. C. Reducing nighttime light exposure in the urban environment to benefit human health and society. Science 380, 1130–1135 (2023).
-
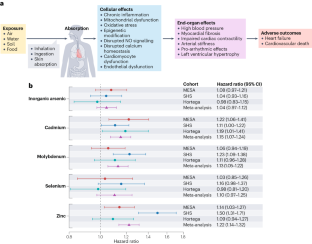
Martinez-Morata, I. et al. Associations between urinary metal levels and incident heart failure: a multi-cohort analysis. JACC Heart Fail. 13, 102510 (2025).
-
Lamas, G. A. et al. Contaminant metals as cardiovascular risk factors: a scientific statement from the American Heart Association. J. Am. Heart Assoc. 12, e029852 (2023).
-
Hahad, O., Al-Kindi, S., Lelieveld, J., Münzel, T. & Daiber, A. Supporting and implementing the beneficial parts of the exposome: the environment can be the problem, but it can also be the solution. Int. J. Hyg. Environ. Health 255, 114290 (2024).
-
Zhang, K., Brook, R. D., Li, Y., Rajagopalan, S. & Kim, J. B. Air pollution, built environment, and early cardiovascular disease. Circ. Res. 132, 1707–1724 (2023).
-
Rajagopalan, S. et al. The urban environment and cardiometabolic health. Circulation 149, 1298–1314 (2024).
-
Ji, L.-D., Tang, N. L. S., Xu, Z. F. & Xu, J. Genes regulate blood pressure, but “environments� cause hypertension. Front. Genet. 11, 580443 (2020).
-
Øvretveit, K. et al. Polygenic interactions with environmental exposures in blood pressure regulation: the HUNT study. J. Am. Heart Assoc. 13, e034612 (2024).
-
Keaton, J. M. et al. Genome-wide analysis in over 1 million individuals of European ancestry yields improved polygenic risk scores for blood pressure traits. Nat. Genet. 56, 778–791 (2024).
-
Pazoki, R. et al. Genetic predisposition to high blood pressure and lifestyle factors: associations with midlife blood pressure levels and cardiovascular events. Circulation 137, 653–661 (2018).
-
Wu, H., Eckhardt, C. M. & Baccarelli, A. A. Molecular mechanisms of environmental exposures and human disease. Nat. Rev. Genet. 24, 332–344 (2023).
-
Baccarelli, A., Dolinoy, D. C. & Walker, C. L. A precision environmental health approach to prevention of human disease. Nat. Commun. 14, 2449 (2023).
-
Tanwar, V. et al. PM2.5 exposure in utero contributes to neonatal cardiac dysfunction in mice. Environ. Pollut. 230, 116–124 (2017).
-
Tanwar, V. et al. In utero particulate matter exposure produces heart failure, electrical remodeling, and epigenetic changes at adulthood. J. Am. Heart Assoc. 6, e005796 (2017).
-
Ho, F. K. et al. A proteomics-based approach for prediction of different cardiovascular diseases and dementia. Circulation 151, 277–287 (2025).
-
Government of Canada. Human Health Risk Assessment for Ambient Nitrogen Dioxide https://www.canada.ca/en/health-canada/services/publications/healthy-living/human-health-risk-assessment-ambient-nitrogen-dioxide.html (2016).
-
Public Health England. Associations of Long-term Average Concentrations of Nitrogen Dioxide with Mortality (2018): COMEAP Summary https://www.gov.uk/government/publications/nitrogen-dioxide-effects-on-mortality/associations-of-long-term-average-concentrations-of-nitrogen-dioxide-with-mortality-2018-comeap-summary (2018).
-
United States Environmental Protection Agency. Integrated Science Assessment (ISA) for Oxides of Nitrogen – Health Criteria (Final Report, Jan 2016) https://cfpub.epa.gov/ncea/isa/recordisplay.cfm?deid=310879 (2016).
-
Thurston, G. D. et al. Ischemic heart disease mortality and long-term exposure to source-related components of U.S. fine particle air pollution. Env. Health Perspect. 124, 785–794 (2016).
-
Eminson, K. et al. Does air pollution confound associations between environmental noise and cardiovascular outcomes? — A systematic review. Env. Res. 232, 116075 (2023).
-
Rajagopalan, S. & Landrigan, P. J. Pollution and the heart. N. Engl. J. Med. 385, 1881–1892 (2021).
-
Abohashem, S. et al. A leucopoietic-arterial axis underlying the link between ambient air pollution and cardiovascular disease in humans. Eur. Heart J. 42, 761–772 (2021).
-
Kuntic, M. et al. Differential inflammation, oxidative stress and cardiovascular damage markers of nano- and micro-particle exposure in mice: implications for human disease burden. Redox Biol. 83, 103644 (2025).
-
Wold, L. E. et al. Cardiovascular remodeling in response to long-term exposure to fine particulate matter air pollution. Circ. Heart Fail. 5, 452–461 (2012).
-
Liu, Q. et al. Potential molecular mechanism of cardiac hypertrophy in mice induced by exposure to ambient PM2. 5. Ecotoxicol. Environ. Saf. 224, 112659 (2021).
-
Wu, T. et al. PM2.5-induced programmed myocardial cell death via mPTP opening results in deteriorated cardiac function in HFpEF mice. Cardiovasc. Toxicol. 22, 746–762 (2022).
-
Mills, N. L. et al. Ischemic and thrombotic effects of dilute diesel-exhaust inhalation in men with coronary heart disease. N. Engl. J. Med. 357, 1075–1082 (2007).
-
Langrish, J. P. et al. Altered nitric oxide bioavailability contributes to diesel exhaust inhalation-induced cardiovascular dysfunction in man. J. Am. Heart Assoc. 2, e004309 (2013).
-
Lucking, A. J. et al. Particle traps prevent adverse vascular and prothrombotic effects of diesel engine exhaust inhalation in men. Circulation 123, 1721–1728 (2011).
-
Shah, A. S. et al. Global association of air pollution and heart failure: a systematic review and meta-analysis. Lancet 382, 1039–1048 (2013).
-
Jia, Y. et al. Effect of air pollution on heart failure: systematic review and meta-analysis. Env. Health Perspect. 131, 76001 (2023).
-
Wang, M. et al. Joint exposure to various ambient air pollutants and incident heart failure: a prospective analysis in UK Biobank. Eur. Heart J. 42, 1582–1591 (2021).
-
Bai, L. et al. Exposure to ambient air pollution and the incidence of congestive heart failure and acute myocardial infarction: a population-based study of 5.1 million Canadian adults living in Ontario. Env. Int. 132, 105004 (2019).
-
Ward-Caviness, C. K. et al. Long-term exposure to particulate air pollution is associated with 30-day readmissions and hospital visits among patients with heart failure. J. Am. Heart Assoc. 10, e019430 (2021).
-
Mentias, A. et al. Ambient air pollution exposure and adverse outcomes among medicare beneficiaries with heart failure. J. Am. Heart Assoc. 13, e032902 (2024).
-
Al-Kindi, S. G. et al. Ambient air pollution and mortality after cardiac transplantation. J. Am. Coll. Cardiology 74, 3026–3035 (2019).
-
Vieira, J. L. et al. Respiratory filter reduces the cardiovascular effects associated with diesel exhaust exposure: a randomized, prospective, double-blind, controlled study of heart failure: the FILTER-HF trial. JACC Heart Fail. 4, 55–64 (2016).
-
Vieira, J. L., Guimaraes, G. V., de Andre, P. A., Saldiva, P. H. & Bocchi, E. A. Effects of reducing exposure to air pollution on submaximal cardiopulmonary test in patients with heart failure: analysis of the randomized, double-blind and controlled FILTER-HF trial. Int. J. Cardiol. 215, 92–97 (2016).
-
Rajagopalan, S. et al. Toward heart-healthy and sustainable cities: a policy statement from the American Heart Association. Circulation 149, e1067–e1089 (2024).
-
Hahad, O. et al. Noise and air pollution as risk factors for hypertension: part. I-epidemiology. Hypertension 80, 1375–1383 (2023).
-
Hahad, O. et al. Noise and air pollution as risk factors for hypertension: part. II-pathophysiologic insight. Hypertension 80, 1384–1392 (2023).
-
Münzel, T., Sørensen, M. & Daiber, A. Transportation noise pollution and cardiovascular disease. Nat. Rev. Cardiol 18, 619–636 (2021).
-
Hahad, O. et al. Cerebral consequences of environmental noise exposure. Environ. Int. 165, 107306 (2022).
-
Fu, X. et al. Long-term exposure to traffic noise and risk of incident cardiovascular diseases: a systematic review and dose-response meta-analysis. J. Urban Health 100, 788–801 (2023).
-
Heritier, H. et al. Transportation noise exposure and cardiovascular mortality: a nationwide cohort study from Switzerland. Eur. J. Epidemiol. 32, 307–315 (2017).
-
Vienneau, D. et al. Transportation noise exposure and cardiovascular mortality: 15-years of follow-up in a nationwide prospective cohort in Switzerland. Env. Int. 158, 106974 (2022).
-
Thacher, J. D. et al. Exposure to transportation noise and risk for cardiovascular disease in a nationwide cohort study from Denmark. Env. Res. 211, 113106 (2022).
-
Yang, T. et al. Long-term exposure to road traffic noise and incident heart failure: evidence from UK Biobank. JACC Heart Fail. 11, 986–996 (2023).
-
Seidler, A. et al. Aircraft, road and railway traffic noise as risk factors for heart failure and hypertensive heart disease — a case-control study based on secondary data. Int. J. Hyg. Env. Health 219, 749–758 (2016).
-
Bai, L. et al. Exposure to road traffic noise and incidence of acute myocardial infarction and congestive heart failure: a population-based cohort study in Toronto, Canada. Env. Health Perspect. 128, 87001 (2020).
-
Topriceanu, C. C. et al. Higher aircraft noise exposure is linked to worse heart structure and function by cardiovascular MRI. J. Am. Coll. Cardiol. 85, 454–469 (2025).
-
Davies, H. W., Vlaanderen, J. J., Henderson, S. B. & Brauer, M. Correlation between co-exposures to noise and air pollution from traffic sources. Occup. Env. Med. 66, 347–350 (2009).
-
Gale, J. E. et al. Disruption of circadian rhythms accelerates development of diabetes through pancreatic beta-cell loss and dysfunction. J. Biol. Rhythm. 26, 423–433 (2011).
-
Kurose, T., Yabe, D. & Inagaki, N. Circadian rhythms and diabetes. J. Diabetes Investig. 2, 176–177 (2011).
-
Qian, J., Yeh, B., Rakshit, K., Colwell, C. S. & Matveyenko, A. V. Circadian disruption and diet-induced obesity synergize to promote development of beta-cell failure and diabetes in male rats. Endocrinology 156, 4426–4436 (2015).
-
Gamble, K. L., Berry, R., Frank, S. J. & Young, M. E. Circadian clock control of endocrine factors. Nat. Rev. Endocrinol. 10, 466–475 (2014).
-
Stenvers, D. J., Scheer, F., Schrauwen, P., la Fleur, S. E. & Kalsbeek, A. Circadian clocks and insulin resistance. Nat. Rev. Endocrinol. 15, 75–89 (2019).
-
Cribbet, M. R. et al. Circadian rhythms and metabolism: from the brain to the gut and back again. Ann. N. Y. Acad. Sci. 1385, 21–40 (2016).
-
Masri, S. & Sassone-Corsi, P. The circadian clock: a framework linking metabolism, epigenetics and neuronal function. Nat. Rev. Neurosci. 14, 69–75 (2013).
-
Masri, S., Zocchi, L., Katada, S., Mora, E. & Sassone-Corsi, P. The circadian clock transcriptional complex: metabolic feedback intersects with epigenetic control. Ann. N. Y. Acad. Sci. 1264, 103–109 (2012).
-
Patel, V. R., Eckel-Mahan, K., Sassone-Corsi, P. & Baldi, P. CircadiOmics: integrating circadian genomics, transcriptomics, proteomics and metabolomics. Nat. Methods 9, 772–773 (2012).
-
Zubidat, A. E. & Haim, A. Artificial light-at-night — a novel lifestyle risk factor for metabolic disorder and cancer morbidity. J. Basic Clin. Physiol. Pharmacol. 28, 295–313 (2017).
-
Palanivel, R. et al. Exposure to air pollution disrupts circadian rhythm through alterations in chromatin dynamics. iScience 23, 101728 (2020).
-
Xu, C. et al. Shift work, genetic factors, and the risk of heart failure: a prospective study of the UK biobank. Mayo Clin. Proc. 97, 1134–1144 (2022).
-
Li, X., He, Y., Wang, D. & Momeni, M. R. Chronobiological disruptions: unravelling the interplay of shift work, circadian rhythms, and vascular health in the context of stroke risk. Clin. Exp. Med. 25, 6 (2024).
-
Lane, K. J. et al. Associations between greenness, impervious surface area, and nighttime lights on biomarkers of vascular aging in Chennai, India. Env. Health Perspect. 125, 087003 (2017).
-
Zhang, J. et al. Role of nighttime light in the association between air pollution exposure and cardiovascular disease. J. Am. Heart Assoc. 14, e042835 (2025).
-
Liang, X. et al. Outdoor light at night and mortality in the UK Biobank: a prospective cohort study. Occup. Env. Med. https://doi.org/10.1136/oemed-2023-109036 (2023).
-
Martinez-Morata, I. et al. Association of urinary metals with cardiovascular disease incidence and all-cause mortality in the multi-ethnic study of atherosclerosis (MESA). Circulation 150, 758–769 (2024).
-
McGraw, K. E. et al. Urinary metal levels and coronary artery calcification: longitudinal evidence in the multi-ethnic study of atherosclerosis. J. Am. Coll. Cardiol. 84, 1545–1557 (2024).
-
Paithankar, J. G., Saini, S., Dwivedi, S., Sharma, A. & Chowdhuri, D. K. Heavy metal associated health hazards: an interplay of oxidative stress and signal transduction. Chemosphere 262, 128350 (2021).
-
Borne, Y. et al. Cadmium exposure and incidence of heart failure and atrial fibrillation: a population-based prospective cohort study. BMJ Open 5, e007366 (2015).
-
Peters, J. L., Perlstein, T. S., Perry, M. J., McNeely, E. & Weuve, J. Cadmium exposure in association with history of stroke and heart failure. Env. Res. 110, 199–206 (2010).
-
Vaziri, N. D. Mechanisms of lead-induced hypertension and cardiovascular disease. Am. J. Physiol. Heart Circ. Physiology 295, H454–H465 (2008).
-
Navas-Acien, A., Guallar, E., Silbergeld, E. K. & Rothenberg, S. J. Lead exposure and cardiovascular disease — a systematic review. Env. Health Perspect. 115, 472–482 (2007).
-
Yang, W. Y. et al. Left ventricular structure and function in relation to environmental exposure to lead and cadmium. J. Am. Heart Assoc. 6, e004692 (2017).
-
Bello, K. A. et al. Chronic exposure to mercury increases arrhythmia and mortality post-acute myocardial infarction in rats. Front. Physiol. 14, 1260509 (2023).
-
Xing, X. et al. Association of selenium and cadmium with heart failure and mortality based on the National Health and Nutrition Examination Survey. J. Hum. Nutr. Diet. 36, 1496–1506 (2023).
-
Sears, C. G. et al. Urinary cadmium and incident heart failure: a case-cohort analysis among never-smokers in Denmark. Epidemiology 33, 185–192 (2022).
-
Lieberman-Cribbin, W. et al. Relationship between urinary uranium and cardiac geometry and left ventricular function: the Strong Heart study. JACC Adv. 3, 101408 (2024).
-
Pichler, G. et al. Association of arsenic exposure with cardiac geometry and left ventricular function in young adults. Circ. Cardiovasc. Imaging 12, e009018 (2019).
-
George, C. M. et al. Effect of an arsenic mitigation program on arsenic exposure in American Indian communities: a cluster randomized controlled trial of the community-led Strong Heart Water Study program. Env. Health Perspect. 132, 37007 (2024).
-
Lamas, G. A. et al. Edetate disodium-based chelation for patients with a previous myocardial infarction and diabetes: TACT2 randomized clinical trial. JAMA 332, 794–803 (2024).
-
Ravalli, F. et al. Chelation therapy in patients with cardiovascular disease: a systematic review. J. Am. Heart Assoc. 11, e024648 (2022).
-
Chowdhury, R. et al. Environmental toxic metal contaminants and risk of cardiovascular disease: systematic review and meta-analysis. BMJ 362, k3310 (2018).
-
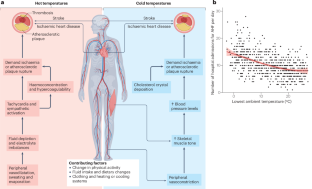
Alahmad, B. et al. Associations between extreme temperatures and cardiovascular cause-specific mortality: results from 27 countries. Circulation 147, 35–46 (2023).
-
Achebak, H. et al. Ambient temperature and risk of cardiovascular and respiratory adverse health outcomes: a nationwide cross-sectional study from Spain. Eur. J. Prev. Cardiol. 31, 1080–1089 (2024).
-
Singh, N. et al. Heat and cardiovascular mortality: an epidemiological perspective. Circ. Res. 134, 1098–1112 (2024).
-
de Schrijver, E. et al. Nationwide projections of heat- and cold-related mortality impacts under various climate change and population development scenarios in Switzerland. Env. Res. Lett. 18, 094010 (2023).
-
Mugele, H. et al. Control of blood pressure in the cold: differentiation of skin and skeletal muscle vascular resistance. Exp. Physiol. 108, 38–49 (2023).
-
Kim, J. & Kim, H. Influence of ambient temperature and diurnal temperature range on incidence of cardiac arrhythmias. Int. J. Biometeorol. 61, 407–416 (2017).
-
Meade, R. D. et al. Meta-analysis of heat-induced changes in cardiac function from over 400 laboratory-based heat exposure studies. Nat. Commun. 16, 2543 (2025).
-
Cui, J. et al. Effects of heat stress on thermoregulatory responses in congestive heart failure patients. Circulation 112, 2286–2292 (2005).
-
Green, D. J. et al. Impaired skin blood flow response to environmental heating in chronic heart failure. Eur. Heart J. 27, 338–343 (2006).
-
Wilker, E. H. et al. Ambient temperature and biomarkers of heart failure: a repeated measures analysis. Env. Health Perspect. 120, 1083–1087 (2012).
-
Qiu, H. et al. Is greater temperature change within a day associated with increased emergency hospital admissions for heart failure? Circ. Heart Fail. 6, 930–935 (2013).
-
Pan, R. et al. Association between ambient temperature and cause-specific cardiovascular disease admissions in Japan: a nationwide study. Env. Res. 225, 115610 (2023).
-
Jimba, T. et al. Association of ambient temperature and acute heart failure with preserved and reduced ejection fraction. ESC Heart Fail. 9, 2899–2908 (2022).
-
Munzel, T. et al. Challenges posed by climate hazards to cardiovascular health and cardiac intensive care: implications for mitigation and adaptation. Eur. Heart J. Acute Cardiovasc. Care 13, 731–744 (2024).
-
Vishram-Nielsen, J. K. et al. Association between the incidence of hospitalizations for acute cardiovascular events, weather, and air pollution. JACC Adv. 2, 100334 (2023).
-
Shih, H.-I. et al. Increased medical visits and mortality among adults with cardiovascular diseases in severely affected areas after Typhoon Morakot. Int. J. Environ. Res. Public Health 17, 6531 (2020).
-
Yan, M. et al. Tropical cyclone exposures and risks of emergency medicare hospital admission for cardiorespiratory diseases in 175 urban United States counties, 1999–2010. Epidemiology 32, 315–326 (2021).
-
Danesh Yazdi, M. et al. The effect of long-term exposure to air pollution and seasonal temperature on hospital admissions with cardiovascular and respiratory disease in the United States: a difference-in-differences analysis. Sci. Total. Env. 843, 156855 (2022).
-
Nieuwenhuijsen, M. J. Green infrastructure and health. Annu. Rev. Public Health 42, 317–328 (2021).
-
Pereira, G. et al. The association between neighborhood greenness and cardiovascular disease: an observational study. BMC Public Health 12, 466 (2012).
-
Yeager, R. et al. Association between residential greenness and cardiovascular disease risk. J. Am. Heart Assoc. 7, e009117 (2018).
-
Dazard, J. E. et al. Association of genetic variants with modifiable environmental factor in cardiovascular disease risk: a UK Biobank Mendelian randomization study. J. Am. Coll. Cardiol 85, a331 (2025).
-
Iyer, H. S. et al. Impact of neighborhood socioeconomic status, income segregation, and greenness on blood biomarkers of inflammation. Env. Int. 162, 107164 (2022).
-
Wang, K. et al. Relationship of neighborhood greenness to heart disease in 249 405 US medicare beneficiaries. J. Am. Heart Assoc. 8, e010258 (2019).
-
Liu, T. et al. Association of neighborhood greenness exposure with cardiovascular diseases and biomarkers. Int. J. Hyg. Env. Health 234, 113738 (2021).
-
Chen, H. et al. Residential greenness and cardiovascular disease incidence, readmission, and mortality. Env. Health Perspect. 128, 87005 (2020).
-
Poulsen, A. H. et al. Concomitant exposure to air pollution, green space, and noise and risk of stroke: a cohort study from Denmark. Lancet Reg. Health Eur. 31, 100655 (2023).
-
Mukhopadhyay, A. et al. Neighborhood-level socioeconomic status and prescription fill patterns among patients with heart failure. JAMA Netw. Open 6, e2347519 (2023).
-
Kowaleski-Jones, L. et al. Walkable neighborhoods and obesity: evaluating effects with a propensity score approach. SSM Popul. Health 6, 9–15 (2017).
-
Son, W. H., Park, H. T., Jeon, B. H. & Ha, M. S. Moderate intensity walking exercises reduce the body mass index and vascular inflammatory factors in postmenopausal women with obesity: a randomized controlled trial. Sci. Rep. 13, 20172 (2023).
-
Yamamoto, Y. et al. Association between subjective walking speed and metabolic diseases in individuals with obesity: a cross-sectional analysis. Sci. Rep. 14, 28228 (2024).
-
Drexel, H. et al. Downhill hiking improves low-grade inflammation, triglycerides, body weight and glucose tolerance. Sci. Rep. 11, 14503 (2021).
-
Marshall, J. D., Brauer, M. & Frank, L. D. Healthy neighborhoods: walkability and air pollution. Environ. Health Perspect. 117, 1752–1759 (2009).
-
Howell, N. A., Tu, J. V., Moineddin, R., Chu, A. & Booth, G. L. Association between neighborhood walkability and predicted 10-year cardiovascular disease risk: the CANHEART (Cardiovascular Health in Ambulatory Care Research Team) cohort. J. Am. Heart Assoc. 8, e013146 (2019).
-
Gorczyca, A. M. et al. Change in physical activity and sitting time after myocardial infarction and mortality among postmenopausal women in the Women’s Health Initiative-Observational study. J. Am. Heart Assoc. 6, e005354 (2017).
-
James, P. et al. Interrelationships between walkability, air pollution, greenness, and body mass index. Epidemiology 28, 780–788 (2017).
-
Appleton, A. A., Holdsworth, E. A. & Kubzansky, L. D. A systematic review of the interplay between social determinants and environmental exposures for early-life outcomes. Curr. Environ. Health Rep. 3, 287–301 (2016).
-
Motairek, I., Chen, Z., Makhlouf, M. H., Rajagopalan, S. & Al-Kindi, S. Historical neighbourhood redlining and contemporary environmental racism. Local. Environ. 28, 518–528 (2023).
-
Al-Kindi, S. et al. Historical neighborhood redlining and cardiovascular risk in patients with chronic kidney disease. Circulation 148, 280–282 (2023).
-
Mentias, A. et al. Historical redlining, socioeconomic distress, and risk of heart failure among medicare beneficiaries. Circulation 148, 210–219 (2023).
-
Fields, N. D. et al. Historical redlining and heart failure outcomes following hospitalization in the Southeastern United States. J. Am. Heart Assoc. 13, e032019 (2024).
-
Calvillo-King, L. et al. Impact of social factors on risk of readmission or mortality in pneumonia and heart failure: systematic review. J. Gen. Intern. Med. 28, 269–282 (2013).
-
Hood, E. Dwelling disparities: how poor housing leads to poor health. Env. Health Perspect. 113, A310–A317 (2005).
-
Zuluaga, M. C. et al. Housing conditions and mortality in older patients hospitalized for heart failure. Am. Heart J. 161, 950–955 (2011).
-
Abohashem, S. et al. Additive effect of high transportation noise exposure and socioeconomic deprivation on stress-associated neural activity, atherosclerotic inflammation, and cardiovascular disease events. J. Expo. Sci. Env. Epidemiol. 35, 62–69 (2025).
-
Dewan, P. et al. Income inequality and outcomes in heart failure: a global between-country analysis. JACC Heart Fail. 7, 336–346 (2019).
-
Tromp, J. et al. Post-discharge prognosis of patients admitted to hospital for heart failure by world region, and national level of income and income disparity (REPORT-HF): a cohort study. Lancet Glob. Health 8, e411–e422 (2020).
-
Hahad, O. et al. Exposomic determinants of atherosclerosis: recent evidence. Curr. Atheroscler. Rep. 27, 28 (2025).
-
Osborne, M. T. et al. The combined effect of air and transportation noise pollution on atherosclerotic inflammation and risk of cardiovascular disease events. J. Nucl. Cardiol. 30, 665–679 (2023).
-
Al-Kindi, S. Leveraging geospatial data science to uncover novel environmental predictors of cardiovascular disease. JACC Adv. 2, 100371 (2023).
-
Ibrahim, R. et al. Big data, big insights: leveraging data analytics to unravel cardiovascular exposome complexities. Methodist. Debakey Cardiovasc. J. 20, 111–123 (2024).
-
Felker, G. M. & Teerlink, J. R. in Braunwald’s Heart Disease: A Textbook of Cardiovascular Medicine 12th edn Ch. 49 (eds Libby, P. et al.) 946–974 (Elsevier, 2022).
-
Zacharias, M., Al-Kindi, S. & Rajagopalan, S. Isolating noise from signals in the air. JACC Heart Fail. 11, 997–999 (2023).
-
Hahad, O. & Al-Kindi, S. Heavy metal, heavy heart: adverse cardiovascular effects of uranium exposure. JACC Adv. 3, 101404 (2024).
-
Bozkurt, B. et al. HF STATS 2024: heart failure epidemiology and outcomes statistics an updated 2024 report from the Heart Failure Society of America. J. Card. Fail. 31, 66–116 (2025).
-
Cho, Y. et al. Effects of artificial light at night on human health: a literature review of observational and experimental studies applied to exposure assessment. Chronobiol. Int. 32, 1294–1310 (2015).
-
Dar, T. et al. Psychosocial stress and cardiovascular disease. Curr. Treat. Options Cardiovasc. Med. 21, 23 (2019).
Acknowledgements
O.H. is a Young Scientist of the DZHK (German Center for Cardiovascular Research), Partner Site Rhine-Main, Mainz, Germany, and Guest Scientist at the Max Planck Institute for Chemistry, Mainz, Germany. The work was supported by the environmental network EXPOHEALTH funded by the Science Initiative of the state Rhineland-Palatinate, Germany, and by the environmental research consortium MARKOPOLO, which is funded by the European Union (Grant Agreement Number 101156161) and the Swiss State Secretariat for Education, Research and Innovation (SERI). S.R. is supported by National Institutes of Health Grant R35 ES031702. The views and opinions expressed are those of the authors only and do not necessarily reflect those of the European Union, the European Health and Digital Executive Agency (HADEA) or the SERI. Neither the European Union nor the granting authorities can be held responsible for them.
Author information
Authors and Affiliations
Contributions
O.H., S.W. and S.A.-K. researched data for the article. O.H., S.W., S.R. and S.A.-K. discussed the content of the manuscript. O.H., S.W. and S.A.-K. wrote the article. All the authors reviewed and edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Cardiology thanks Andreas Daiber and George Thurston for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hahad, O., Wass, S., Rajagopalan, S. et al. The environmental exposome in heart failure risk and progression.
Nat Rev Cardiol (2026). https://doi.org/10.1038/s41569-026-01247-1
-
Accepted:
-
Published:
-
Version of record:
-
DOI: https://doi.org/10.1038/s41569-026-01247-1
Search
RECENT PRESS RELEASES
Related Post